Immunology is a field rich with complex interactions between various components of the immune system. Among the key concepts in this discipline are immunogens, antigens, and epitopes. These terms are foundational for understanding how the immune system detects and responds to foreign substances. Additionally, the Major Histocompatibility Complex (MHC) plays a crucial role in this process. This article provides a detailed exploration of these concepts, focusing particularly on the roles of MHC class I and class II molecules, their functions in immune response, and their comparative aspects.
What is an Immunogen?
An immunogen is a macromolecule capable of eliciting an immune response in an immunocompetent host. This immune response typically involves the production of immunoglobulins (antibodies) or the activation of sensitized lymphocytes. Immunogens are essential in vaccine development and understanding how the body defends itself against pathogens.
Characteristics of Effective Immunogens
- Molecular Size: Larger molecules, generally those with a molecular weight above 10,000 Daltons, are more likely to be immunogenic. Proteins are especially potent immunogens due to their size and structural complexity.
- Complexity: Complex molecules with multiple structural components (e.g., proteins with tertiary or quaternary structures) are more effective at inducing an immune response compared to simple molecules.
- Foreignness: Immunogens need to be perceived as foreign by the immune system. The greater the difference between the immunogen and the host’s own molecules, the stronger the immune response.
- Stability and Dosage: The stability of the immunogen and the dosage at which it is administered can also influence the effectiveness of the immune response.
Differentiating Antigens from Immunogens
While antigens and immunogens are related, they have distinct meanings:
- Antigen: An antigen is a substance that, while not necessarily provoking an immune response on its own, can be specifically recognized and bound by antibodies or T cell receptors once an immune response has been generated. In essence, antigens are the targets of immune responses.
- Immunogen: An immunogen is a substance that actively induces an immune response. All immunogens are antigens, but not all antigens are immunogens.
Factors Influencing Immunogenicity
The effectiveness of an immunogen is influenced by several factors:
- Molecular Weight and Complexity: Larger and more complex molecules are generally better immunogens. For example, proteins with multiple epitopes are more effective at eliciting an immune response than smaller, simpler molecules.
- Age and Health of the Host: The immune response varies with age and health status. Infants, the elderly, and immunocompromised individuals may respond differently to immunogens.
- Genetic Makeup: Genetic variations can affect immune response efficiency. For instance, certain genetic profiles can enhance or diminish an individual’s response to specific immunogens.
- Route of Inoculation: The method of introducing an immunogen (e.g., intravenous, oral, or subcutaneous) affects the nature and intensity of the immune response.
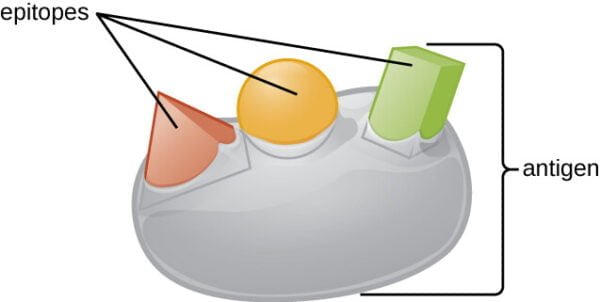
Understanding Epitopes
An epitope is the specific part of an antigen that is recognized by the immune system. Epitopes can be classified into:
- Linear Epitopes: Composed of a linear sequence of amino acids within a protein. These epitopes are recognized by antibodies or T cell receptors based on their specific sequence.
- Conformational Epitopes: Formed by the three-dimensional folding of a protein. These epitopes are recognized based on the overall structure of the protein, not just its linear sequence.
Haptens and Their Role in Immunology
Haptens are small molecules that are not immunogenic by themselves. However, when attached to a larger carrier molecule, they can induce an immune response. This conjugation allows the immune system to recognize the hapten as part of a larger, foreign entity.
Examples of Haptens
- Penicillin: In some individuals, penicillin acts as a hapten by binding to proteins in the body, potentially leading to an allergic reaction.
- Poison Ivy: The chemical urushiol in poison ivy acts as a hapten. When it binds to skin proteins, it can trigger an allergic response known as contact dermatitis.
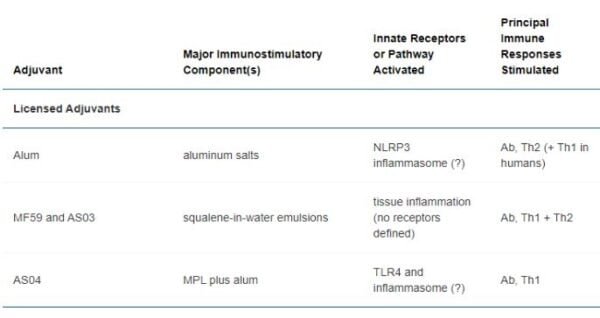
The Role of Adjuvants in Enhancing Immune Response
Adjuvants are substances that enhance the immune response to an antigen. They work by stimulating the immune system or by increasing the immunogenicity of the antigen.
Types of Adjuvants
- Alum (Aluminum Salts): Used in many vaccines, alum precipitates antigens, allowing for a prolonged exposure to the immune system and thereby enhancing the immune response.
- Oil-in-Water Emulsions: Create a depot effect, which slowly releases the antigen over time, boosting the immune response.
- Toll-Like Receptor Agonists: Mimic pathogen-associated molecular patterns to stimulate the innate immune system, which in turn enhances the adaptive immune response.
Types of Antigens
Antigens can be categorized based on their origin:
- Autoantigens: These are self-antigens that belong to the host. In autoimmune diseases, the immune system mistakenly targets these autoantigens as foreign, leading to conditions such as rheumatoid arthritis or lupus.
- Alloantigens: These are antigens from the same species as the host but are not identical. They are crucial in contexts like blood transfusions and organ transplants, where matching donor and recipient antigens is important to avoid rejection.
- Heteroantigens: These originate from different species and are recognized as foreign by the immune system. For example, bacterial and viral antigens can trigger immune responses.
- Heterophile Antigens: Found in unrelated species but share structural similarities. For instance, some antibodies can cross-react with similar antigens in different species, leading to unexpected immune reactions.
Major Histocompatibility Complex (MHC) and Its Classes
The Major Histocompatibility Complex (MHC) is a set of molecules displayed on cell surfaces that are essential for antigen presentation to T cells. The MHC is divided into two main classes:
Class I MHC Molecules
Class I MHC molecules are present on almost all nucleated cells. They play a critical role in presenting endogenous antigens (proteins synthesized within the cell) to CD8+ T cells, which are cytotoxic T cells. The key functions and characteristics of Class I MHC molecules include:
- Presentation of Endogenous Antigens: Class I MHC molecules bind peptides derived from proteins synthesized within the cell and present them to CD8+ T cells. This process allows the immune system to recognize and eliminate cells infected by viruses or transformed by cancer.
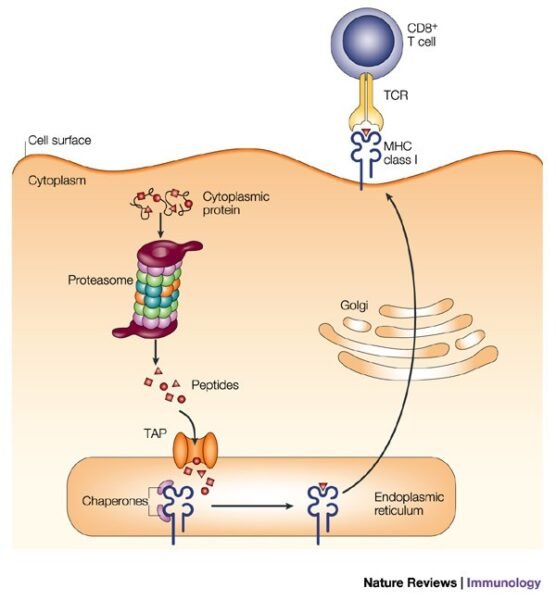
- Structure: Class I MHC molecules consist of a heavy chain (alpha chain), a light chain (beta-2 microglobulin), and a peptide binding groove. The heavy chain is anchored in the cell membrane and forms a complex with beta-2 microglobulin.
- Activation of Cytotoxic T Cells: The interaction between Class I MHC-peptide complexes and CD8+ T cells triggers cytotoxic reactions, leading to the destruction of infected or abnormal cells.
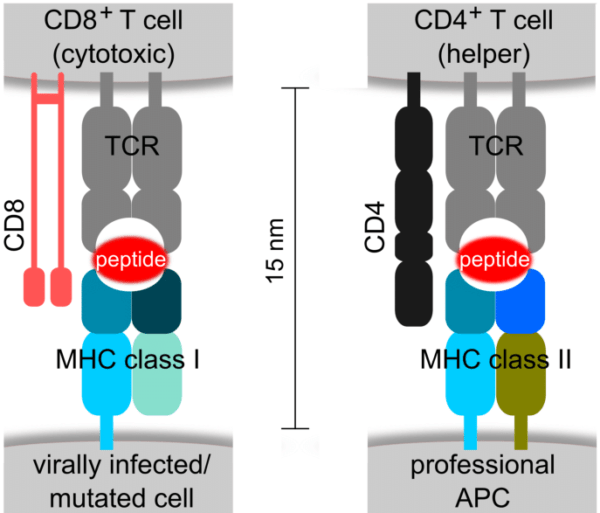
Class II MHC Molecules
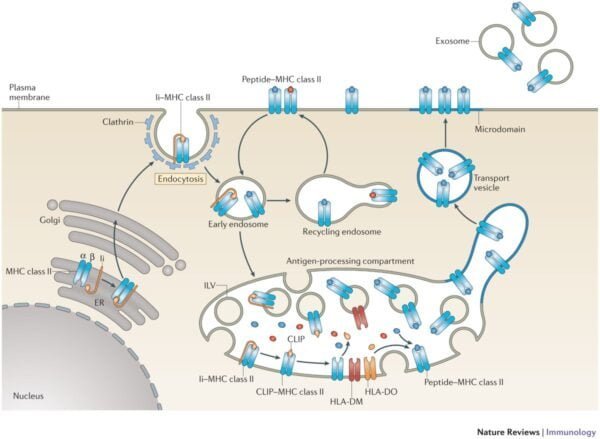
Class II MHC molecules are expressed primarily on professional antigen-presenting cells (APCs) such as dendritic cells, macrophages, and B cells. They are responsible for presenting exogenous antigens (derived from outside the cell) to CD4+ T cells, also known as T helper cells. Key aspects of Class II MHC molecules include:
- Presentation of Exogenous Antigens: Class II MHC molecules bind peptides derived from extracellular proteins that have been processed and presented by APCs. These peptides are presented to CD4+ T cells, which play a crucial role in coordinating the immune response.
- Structure: Class II MHC molecules consist of two alpha and two beta chains, forming a peptide binding groove. Both chains are integral to the cell membrane and work together to bind and present peptides.
- Activation of T Helper Cells: The interaction between Class II MHC-peptide complexes and CD4+ T cells stimulates the production of cytokines, which helps in activating B cells and other immune cells, thereby enhancing the overall immune response.
Comparative Aspects of MHC Class I and Class II
While both Class I and Class II MHC molecules are involved in antigen presentation, they differ in several key ways:
- Antigen Source: Class I MHC molecules present endogenous antigens (e.g., from intracellular pathogens or cancer cells), whereas Class II MHC molecules present exogenous antigens (e.g., from extracellular pathogens that have been internalized and processed by APCs).
- Cell Type Expression: Class I MHC molecules are found on nearly all nucleated cells, allowing for widespread surveillance of intracellular content. Class II MHC molecules are primarily expressed on APCs, focusing on the presentation of processed external antigens.
- T Cell Interaction: Class I MHC molecules interact with CD8+ T cells, which are primarily involved in cytotoxic responses. In contrast, Class II MHC molecules interact with CD4+ T cells, which assist in orchestrating the immune response through cytokine release and support for B cells.
Human Leukocyte Antigen (HLA) System
The Human Leukocyte Antigen (HLA) system is a highly polymorphic set of molecules within the MHC that plays a crucial role in immune recognition. The HLA system includes:
- HLA Class I: Includes HLA-A, HLA-B, and HLA-C. These molecules present endogenous antigens to CD8+ T cells and are involved in recognizing and eliminating infected or malignant cells.
- HLA Class II: Includes HLA-DP, HLA-DQ, and HLA-DR. These molecules present exogenous antigens to CD4+ T cells and are involved in regulating the immune response and assisting in antibody production.
HLA and Disease Associations
Certain HLA types are linked to specific autoimmune diseases:
- HLA-B27: Associated with ankylosing spondylitis and other spondyloarthropathies. The presence of HLA-B27 increases susceptibility to these conditions.
- HLA-DR4: Linked to rheumatoid arthritis and type 1 diabetes. Specific HLA-DR4 alleles are associated with a higher risk of developing these autoimmune disorders.
HLA typing is crucial for organ transplantation, as matching donor and recipient HLA types can reduce the risk of transplant rejection. Additionally, HLA profiles can provide insights into disease susceptibility and guide personalized medical interventions.
Conclusion
The study of immunogens, antigens, and the Major Histocompatibility Complex provides a comprehensive understanding of how the immune system detects and responds to foreign substances. Class I and Class II MHC molecules play distinct but complementary roles in antigen presentation, enabling the immune system to effectively recognize and combat various pathogens and abnormal cells. The HLA system further emphasizes the complexity of immune recognition and its implications for disease and transplantation.
By exploring these concepts in detail, we gain valuable insights into the mechanisms underlying immune responses and the potential for therapeutic interventions. Continued research and advancements in immunology promise to enhance our understanding and treatment of immune-related conditions, ultimately improving health outcomes and quality of life.
References
- Janeway, C. A., Travers, P., Walport, M., & Shlomchik, M. J. (2001). Immunobiology: The Immune System in Health and Disease (5th ed.). Garland Science.
- Alberts, B., Johnson, A., Lewis, J., Raff, M., Roberts, K., & Walter, P. (2002). Molecular Biology of the Cell (4th ed.). Garland Science.
- Horton, R., Wilming, L. G., Rand, V., Lovering, R. C., Bruford, E. A., Khodiyar, V., & Dunn, M. (2004). “Gene map of the extended human MHC.” Nature Reviews Genetics, 5(12), 889-899. doi:10.1038/nrg1495
- Klein, J., & Sato, A. (2000). “The HLA system.” Immunity, 12(3), 241-247. doi:10.1016/S1074-7613(00)80140-5
- Rosenberg, S. A., & Restifo, N. P. (2015). “Adoptive cell transfer as personalized immunotherapy for human cancer.” Science, 348(6230), 62-68. doi:10.1126/science.aaa4967