Adaptive immunity is a key part of our immune system that helps us fight off infections in a specific and lasting way. Unlike our body’s first line of defense, which works quickly but generally, adaptive immunity takes a bit longer to kick in but is much more precise. It involves two main types of immune cells: T-cells and B-cells. These cells not only remember past infections but also react more effectively if the same pathogen invades again. In this guide, we’ll break down how adaptive immunity works, focusing on how T-cells and B-cells develop and contribute to our immune responses. Whether you’re curious about how your body fights diseases or just looking to learn more, this article will give you a clear understanding of how adaptive immunity protects you.
Introduction to Adaptive Immunity
Adaptive immunity, also known as acquired immunity, represents a sophisticated defense system designed to recognize and eliminate specific pathogens or antigens. Unlike innate immunity, which provides a broad and general defense against a wide range of invaders, adaptive immunity offers targeted responses and retains a memory of previous encounters with specific antigens. This memory allows the immune system to respond more rapidly and effectively upon subsequent exposures to the same pathogen.
Characteristics of Adaptive Immunity
Adaptive immunity is distinguished by several key characteristics:
- Specificity: This system is highly specific to individual microbes and pathogens. It achieves this specificity through the diverse repertoire of antigen receptors on lymphocytes, which enables the immune system to precisely target a vast array of antigens.
- Memory: One of the most distinctive features of adaptive immunity is its ability to remember prior exposures to antigens. After the immune system encounters a pathogen, it generates memory cells that persist long-term. Upon reexposure to the same antigen, these memory cells facilitate a more rapid and robust immune response.
- Enhanced Response: Following an initial exposure to a pathogen, the immune response becomes quicker and more effective during subsequent encounters. This enhancement is due to the memory component, which allows for a more efficient clearance of the pathogen.
Adaptive immunity typically takes longer to become activated compared to innate immunity but provides a more enduring protection. The immune system utilizes two main branches to achieve this: cell-mediated immunity and humoral immunity.
T-Cell Differentiation and Function
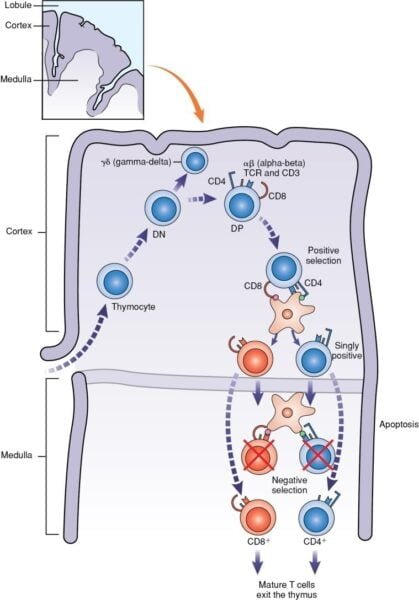
T-Cell Development
T cells originate from hematopoietic stem cells in the bone marrow and mature in the thymus. Their development is a multi-stage process:
- Double Negative (DN) Stage: At this early stage, thymocytes lack both CD4 and CD8 surface markers.
- Double Positive (DP) Stage: Thymocytes express both CD4 and CD8 markers as they undergo gene rearrangement for the T-cell receptor (TCR).
- Single Positive (SP) Stage: Thymocytes that successfully rearrange their TCR genes and pass selection processes express either CD4 or CD8, but not both.
During their time in the thymus, thymocytes go through several crucial processes:
- Gene Rearrangement: Thymocytes undergo rearrangement of genes coding for the beta chain of the TCR, resulting in a unique antigen-binding site.
- Positive Selection: Thymocytes are selected based on their ability to moderately recognize MHC molecules on stromal cells in the thymic cortex. Successful thymocytes proceed to the next stage.
- Negative Selection: Thymocytes that either fail to bind MHC molecules or bind too strongly to self-antigens undergo apoptosis, ensuring self-tolerance and preventing autoimmunity.
T-Cell Subsets and Functions
T cells can be categorized into several subsets based on their surface markers and functions:
- Helper T Cells (CD4+): These cells assist other immune cells by secreting cytokines. They are further divided into:
- Th1 Cells: Produce cytokines such as IFN-γ, IL-2, and TNF-β. They are essential for activating cytotoxic T cells (Tc) and macrophages to combat intracellular pathogens.
- Th2 Cells: Secrete interleukins IL-4, IL-5, IL-6, IL-9, IL-10, and IL-13. Th2 cells help B cells produce antibodies and are involved in the clearance of extracellular parasites and allergic responses.
- Th17 Cells: Produce IL-17 and IL-22, recruiting granulocytes to fight bacterial infections and potentially contributing to autoimmune diseases.
- Regulatory T Cells (Tregs, CD4+CD25+): These cells help maintain immune tolerance by suppressing the immune response to self-antigens and harmless antigens. They secrete inhibitory cytokines to modulate the activity of other T-cell populations.
- Cytotoxic T Cells (CD8+): These cells are specialized in killing cells infected with intracellular pathogens. They release cytotoxic granules containing perforin and granzymes and can induce apoptosis in target cells through the engagement of death receptors.
B-Cell Differentiation and Function
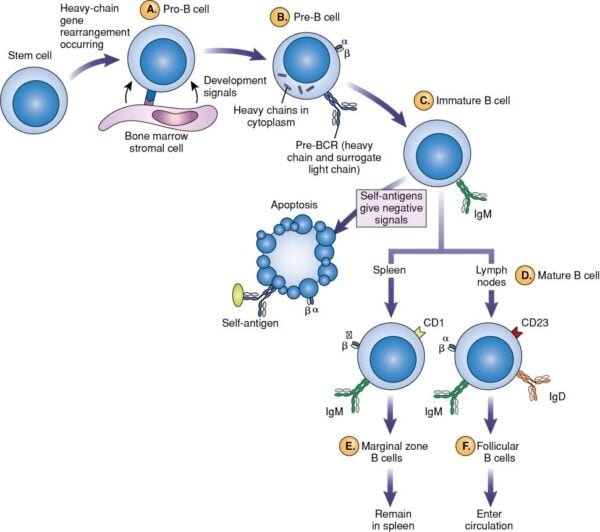
B-Cell Development
B cells also originate from hematopoietic stem cells but mature in the bone marrow. Their development includes several stages:
- Antigen-Independent Phase: This occurs in the bone marrow and involves progression through:
- Pro-B Cells: Begin to rearrange immunoglobulin genes.
- Pre-B Cells: Express a pre-B cell receptor (pre-BCR) with a heavy chain and a surrogate light chain.
- Immature B Cells: Complete rearrangement of light chain genes, expressing a functional B-cell receptor (BCR) on their surface.
- Mature B Cells: Have functional BCRs and are ready to migrate to secondary lymphoid organs.
During development, B cells undergo gene rearrangement to produce a diverse repertoire of antibody specificities. This process includes the creation of variable regions through somatic recombination, essential for recognizing a broad range of antigens.
Antigen-Dependent Phase
Upon encountering an antigen, B cells enter the antigen-dependent phase:
- Activation and Proliferation: B cells are activated upon binding to their specific antigen. This activation often requires assistance from Th cells, especially for T-dependent antigens. B cells then proliferate and differentiate.
- Differentiation: Activated B cells differentiate into:
- Plasma Cells: Specialized in producing and secreting large quantities of antibodies. They are found in bone marrow and peripheral lymphoid organs, having abundant cytoplasmic immunoglobulins (Ig) but little surface Ig.
- Memory B Cells: Persist long-term and can respond more rapidly and effectively to subsequent exposures to the same antigen.
Role of T Cells in Adaptive Immune Response
T cells are crucial in the adaptive immune response through their interactions with antigen-presenting cells (APCs) and their differentiation into various subsets:
- APCs: These include dendritic cells, macrophages, and B cells. APCs process and present antigen fragments to T cells via MHC molecules, which is essential for initiating the adaptive immune response.
- T-Cell Activation: T cells circulate through the bloodstream, lymph nodes, and secondary lymphoid tissues in search of APCs presenting specific antigen-MHC complexes. The interaction between the TCR and antigen-MHC complex, along with additional co-stimulatory signals, leads to T-cell activation and proliferation.
Role of B Cells in Adaptive Immune Response
B cells are central to the humoral immune response:
- Antigen Recognition and Binding: B cells have membrane-bound immunoglobulins that act as antigen receptors. Upon encountering an antigen, B cells undergo activation and differentiation.
- Production of Antibodies: Activated B cells differentiate into plasma cells that secrete antibodies. These antibodies neutralize pathogens, promote phagocytosis, and activate the complement system.
T-Dependent and T-Independent Antigens
- T-Dependent Antigens: These antigens require the help of T helper cells for B-cell activation. B cells respond by producing various antibody classes (e.g., IgG) and generating memory cells. The antigen specificity of the BCR improves during the immune response through a process known as affinity maturation.
- T-Independent Antigens: These antigens can activate B cells without T cell help. They typically have repetitive structures that cross-link BCRs, leading to the production of IgM antibodies. However, T-independent responses generally do not generate memory cells.
Clinical Implications and Advances
Autoimmune Diseases
Failures in adaptive immunity can lead to autoimmune diseases, where the immune system mistakenly targets self-tissues. Examples include:
- Rheumatoid Arthritis: Characterized by chronic inflammation of the joints.
- Type 1 Diabetes: Involves the destruction of insulin-producing cells in the pancreas.
Immunodeficiencies
Immunodeficiencies result from defects in adaptive immunity, leading to increased susceptibility to infections. Examples include:
- Severe Combined Immunodeficiency (SCID): A genetic disorder leading to a severe lack of both B and T cells.
- HIV/AIDS: Human Immunodeficiency Virus targets CD4+ T cells, leading to acquired immunodeficiency.
Advances in Immunotherapy
Recent advances in immunology have led to innovative treatments such as:
- CAR-T Cell Therapy: Involves engineering patients’ T cells to express chimeric antigen receptors (CARs) targeting cancer cells.
- mRNA Vaccines: Utilize messenger RNA to instruct cells to produce antigens, leading to an immune response. This technology has been notably applied in COVID-19 vaccines.
Conclusion
Adaptive immunity is a complex and highly specialized system that provides targeted and long-lasting protection against specific pathogens. Through the intricate processes of T-cell and B-cell development, activation, and differentiation, the adaptive immune system ensures a precise response to infections and the ability to remember previous encounters. Understanding these mechanisms not only enhances our knowledge of immune function but also informs the development of novel therapies and vaccines, highlighting the crucial role of adaptive immunity in maintaining health and combating disease.
References
- Janeway, C. A., Travers, P., Walport, M., & Shlomchik, M. J. (2001). Immunobiology: The Immune System in Health and Disease (5th ed.). Garland Science.
- Murphy, K., & Weaver, C. (2016). Janeway’s Immunobiology (9th ed.). Garland Science.
- Alberts, B., Johnson, A., Lewis, J., Raff, M., Roberts, K., & Walter, P. (2002). Molecular Biology of the Cell (4th ed.). Garland Science.
- Kumagai, Y., & Takeuchi, O. (2014). “The Role of Pattern Recognition Receptors in Innate Immunity and Adaptive Immunity.” Current Opinion in Immunology, 26, 1-8.
- Banchereau, J., & Steinman, R. M. (1998). “Dendritic Cells and the Control of Immunity.” Science, 296(5573), 294-298.
- Nijmegen, R. M., & Tanaka, T. (2020). “The Development and Function of Regulatory T Cells.” Annual Review of Immunology, 38, 177-204.
- Galli, S. J., Nakae, S., & Tsai, M. (2005). “Mast Cells in the Development of Allergic Disease.” Nature Reviews Immunology, 5(7), 573-585.
- Sok, D., & Burton, D. R. (2018). “Recent Advances in Antibody-Based Therapies.” Nature Reviews Drug Discovery, 17(6), 441-458.