Author : Roshni NepalPhylum – Sarcomastigophora
Sub- phylum – Sarcodina
Class – Lobosea
Genus – Entamoeba
Species – histolytica
Several protozoan species in the genus Entamoeba colonize humans, but not all of them are associated with disease. Entamoeba histolytica is well recognized as a pathogenic amoeba (60µm in size), associated with intestinal and extraintestinal infections. Infections are caused due to ingestion of mature quadrinucleate cysts from fecally contaminated food, water or hands.
Habitat and geographical distribution
The parasite resides in the large intestine or lumen of the colon, in host body. Infection is more common in warmer areas, but this is because of both poorer hygiene and the parasitic cysts surviving longer in warm moist conditions.Since amoebiasis is transmitted through contaminated food and water, it is often endemic in regions of the world with limited modern sanitation systems, including México, Central America, western South America, South Asia, and western and southern Africa.
Life cycle of E. histolytica
Cysts and trophozoites are passed in feces. Cysts are typically found in formed (slightly hard) stool, whereas trophozoites are typically found in diarrheal(watery) stool. Infection by Entamoeba histolytica occurs by ingestion of mature cysts in fecally contaminated food, water, or hands. Excystation occurs in the small intestine and trophozoites are released, which migrate to the large intestine. The trophozoites multiply by binary fission and produce cysts, and both stages are passed in the feces. Because of the protection conferred/provided by their walls, the cysts can survive days to weeks in the external environment and are responsible for transmission. Trophozoites passed in the stool are rapidly destroyed once outside the body, and if ingested would not survive exposure to the gastric environment. In many cases, the trophozoites remain confined to the intestinal lumen of individuals who are asymptomatic carriers, passing cysts in their stool (noninvasive infection phase). In some patients the trophozoites invade the intestinal mucosa (intestinal disease phase), or, through the bloodstream, extraintestinal sites such as the liver, brain, and lungs (extraintestinal disease phase), which may lead to amoebic hepatitits, and amoebic liver abscesses. Under unfavourable condition, the trophozoites in large intestine convert in quadrinucleate cyst (encystation), which are passed out in the environment and the life cycle continues.
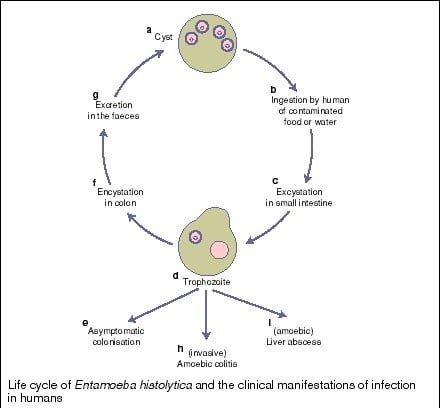
Fig – Life cycle of E. histolytica
Clinical manifestation of amoebiasis
Amoebiasis results from tissue destruction caused induced by E. histolytica. It secretes a proteolytic enzyme called histolysin,that results in tissue destruction and forming a flask-shaped ulcer. After incubation period of (1-4) weeks, infection can result in 3 different forms;
a. Asymptomatic / non – invasive infection –
the carrier of the parasite (host) continually passes cyst in their stool, without getting infected.
b. Intestinal infection –
due to the invasion of colon lining of the intestine, lesions/ulcers are formed. This might result in bloody diarrhea and dysentery with abdominal pain.
c. Extra- intestinal infection –
in some cases, the trophozoites of the parasite after reaching the intestine, through the bloodstream, might invade extraintestinal sites like liver, lungs and brain and result in abscess formation in these area. Amoebic appendicitis is also found in some cases.
Laboratory diagnosis
i. Macroscopy – direct or gross appearance of stool is formed and consist of mucus and blood.
ii. Stool examination – human infections are usually diagnosed by finding cysts and trophozoites shed in the stool. Wet mount, normal saline and Lugol’s iodine preparation can be used for cyst detection in the sample.Since cysts are not shed constantly, a minimum of three stools are examined
iii. Serologic tests- detection of antibody against E. histolytica in blood. Using serum, following tests can be done to carry out the serologic test-
ELISA, IHA, Counter electrophoresis, Immunofluorescence assay (IFA) iv. Liver biopsy – trophozoite stage of parasite can be observed.
v. Pus aspiration from liver – sample should be observed immediately with a drop of warm saline on a microscopic slide. Pus consists of lysed liver cells, RBC and WBC. It has a red – brown achovy sauce appearance.
vi. PCR
Treatment, prevention and control
Those with symptoms require treatment with three medications, an amoebicidal tissue-active agent (Metronidazole, Tinidazole) and a luminal cysticidal agent (Diloxanade) and one that is only effective in liver (Chloroquine).
•To help prevent the spread of amoebiasis around the home (personal prophylaxis):
- Wash hands thoroughly with soap and hot running water for at least 10 seconds after using the toilet or changing a baby’s diaper, and before handling food.
- Clean bathrooms and toilets often; pay particular attention to toilet seats and taps.
- Avoid sharing towels or face washers.
•To help prevent infection (community prophylaxis):
- Avoid raw vegetables when in endemic areas, as they may have been fertilized using human feces.
- Boil water or treat with iodine tablets.
- Avoid eating street foods especially in public places where others are sharing sauces in one container