Placenta previa is defined as a condition in which placenta is implanted partially over the lower uterine segment. About 35% of cases of antepartum hemorrhage is due to placenta previa and it’s incidence ranges from 0.5 to 1% amongst hospital deliveries. Multiparous women are at high risk of developing it. Women beyond 35 years, with high birth order pregnancies and multiple pregnancies are at high risk of developing placenta previa.
Theories postulated for placenta previa
- Dropping Down Theory: Fertilized ovum drops down and implants in the lower uterine segment.
- Persistence of Chorionic Activity: Lesser degree of previa associated with chorionic activity.
- Defective Decidua: Wide-spread decidua causes membranous placenta intrusion.
- Big Surface Area: Large placental surface contributes to the condition.
High-Risk Factors
- Multiparity
- Maternal age > 35 years
- Asian ethnicity, especially women from Mainland China
- Previous cesarean section, myomectomy, hysterotomy
- Prior curettage and placenta previa
- Multiple pregnancies
- Smoking and drug use
Pathological changes in placenta and umbilical cord
Large and thin placenta with extensive areas of degeneration with calcification and infarction. Placenta may be morbidly adherent to lower segment.
Attachment of umbilical cord may be at margin or into the membranes and the insertion may be close to internal os.
Types of placenta previa
Type 1: Low-lying
Only small part of placenta encroaches towards the lower segment but doesn’t reach the internal os.
Type 2: Marginal
The placenta does not cover internal os but reaches the margin of it.
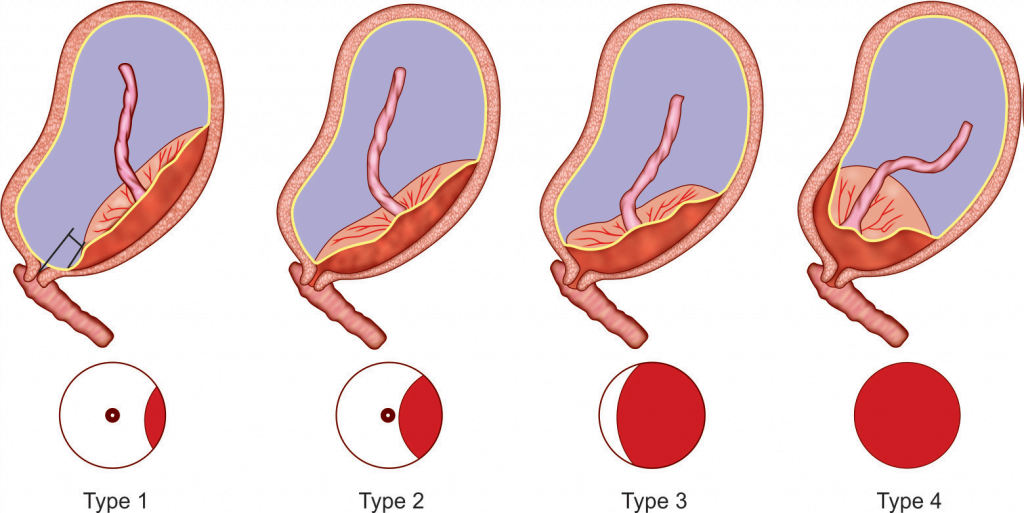
Type 3: Incomplete or partial central
The placenta covers the internal os partially.
Type 4: Central or complete
The placntacompletely overs the internal os even after os is fully dilated.
Differentiating Minor & Major Cases
- Minor: Placenta lies in the lower segment but doesn’t cover the internal os.
- Major: Placenta lies in the lower segment and covers the internal os.
Presentations of Placenta prevue
Vaginal bleeding is the only symptom of which is of sudden onset, painless, apparently causeless and recurrent. Bleeding usually occurs at night and awakening the patient in a pool a blood and majority occurs before 38 weeks.
What findings are seen in Placenta Previa?
- The size of uterus is as that of usual period of gestation, and it is relaxed, soft and elastic without any localized tenderness.
- Increase incidence of malpresentation and multiple pregnancy.
- Head is not fixed and usually floating and cannot be pushed down into the pelvis.
- Fetal heart sound is usually present.
- Bright red or dark colored blood is seen on vulval inspection.
- Vaginal examination is avoided.
Investigations
- Ultrasonography (transabdominal, transvaginal, transperineal)
- Three-dimensional power Doppler
- MRI
Confusable Conditions
- Abruptio placenta
- Cervical polyp, carcinoma
Complications of Placenta previa
Maternal:
- Antepartum hemorrhage
- Early rupture of membranes
- Intrapartum and postpartum hemorrhage
- Infection risks
Fetal:
- Fetal growth retardation
- Low birth weight
- Cord prolapse
- Asphyxia
- Birth injuries
- Intrauterine death
- Congenital malformation
- Embolism
Management:
Management not only include treatment but also prevention to minimize the risk.
Prevention of Placenta previa
- Regular antenatal check-up and early confirmation of diagnosis.
Management at home:
- Patient is put to bed and proper assessment of blood loss.
- Gentle examination of abdomen to assess height of uterus and assess fetal heart sound.
- Avoid vaginal examination.
- Arrangement should be made to transfer patient to hospital well equipped with facility of blood transfusion, cesarean section, and proper neonatal case with intensive unit.
Hospital admission
- All cases of antepartum hemorrhage should be admitted to hospital.
Treatment at hospital
- First patient should be assessed for amount of blood loss.
- A large-bore IV canula is opened and blood is sent for blood grouping, cross-matching and hemoglobin estimation.
- Infusion of normal saline.
- Gentle examination of abdomen and vulval examination is done.
- Diagnosis is made.
Expectant management :
Macaffee regime:
Carry pregnancy till term for fetal lung maturation without putting mother at risk.
It should be continued until 37 weeks, but can be terminated immediately if patient rebleeds.
Indications:
- No active bleeding
- Patient is hemodynamically stable
- Period of gestation is less than 37 weeks
- Reactive cardiotocography
- Absent of fetal anomalies
Active management:
To terminate pregnancy irrespective of period of gestation.
Indications:
- Hemodynamically unstable and active bleeding
- Gestational age more than 37 weeks and in labor
- Fetal distress
- Fetal anomalies present
Mode of delivery :
It depends on types of placenta previa.
- Minor degree of p. previa ( Type 1 and type 2 anterior ): Vaginal delivery is tried.
- Dangerous variety ( Type 2 posterior ): Cesarean section is done.
- Major degree (Type 3 or type 4 ): Cesarean section is done.
Prognosis
- In developed countries, maternal death is decreased to less tha 1% or even to zero in some centers.
- In developing countries, maternal mortality in hospital statistics is as high as 5%.
- Perinatal mortality ranges from 10% to 25%.
References:
- DC Dutta’s Textbook of OBSTETRICS; 9th Edition
- William’s Obstetrics 24th Edition
- https://www.ncbi.nlm.nih.gov/books/NBK539818/
- https://pubmed.ncbi.nlm.nih.gov/23551357/
- https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg27/
- Karami, M., & Jenabi, E. (2017). Placenta previa after prior abortion: a meta-analysis. Biomedical Research and Therapy, 4(07), 1441-1450. https://doi.org/10.15419/bmrat.v4i07.197