Gram staining is a cornerstone technique in microbiology, crucial for differentiating between two major groups of bacteria based on their cell wall properties. Developed by Hans Christian Gram in 1882, this staining method has become a standardized protocol used in laboratories worldwide. In this comprehensive guide, we delve into the intricate details of the Gram staining protocol, exploring its principle, procedure, and significance in microbiological diagnostics.
What is a Gram Stain?
Gram stain is a laboratory test conducted to identify bacteria present in samples obtained from suspected infection sites or bodily fluids. It involves applying a series of dyes to the sample, leading to the visualization of bacteria under a microscope. The staining process helps categorize bacteria as either Gram-positive or Gram-negative based on their reaction to the staining.
Principle of Gram Staining:
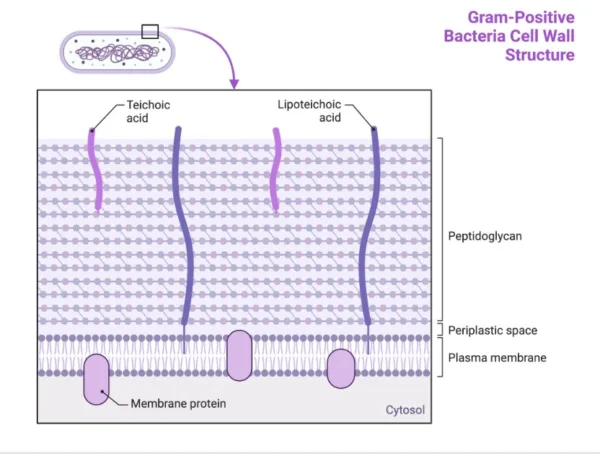
The Gram staining exploits the differences in the structure and composition of bacterial cell walls to categorize them into two distinct groups: Gram-positive and Gram-negative.
- Gram-Positive Bacteria: These bacteria possess a thick layer of peptidoglycan in their cell walls, which retains the crystal violet dye during staining, imparting a purple-blue color.
- Gram-Negative Bacteria: In contrast, Gram-negative bacteria have a thinner peptidoglycan layer and an outer lipid membrane. During staining, they lose the crystal violet dye but are counterstained with a red dye, appearing pink or red under the microscope.

Gram staining Procedure
The Gram staining involves a series of steps:
1. Sample Preparation:
- Apply a small amount of the sample, obtained from the suspected infection site or bodily fluid, onto a clean microscope slide.
- Heat fix the slide by passing it through a Bunsen burner flame several times. This process ensures that the sample adheres firmly to the slide.
2. Staining Process:
a. Application of Crystal Violet:
- Flood the heat-fixed sample with crystal violet solution, covering the entire slide.
- Allow the crystal violet to stand for a specified duration, typically around one minute.
b. Addition of Gram’s Iodine Solution:
- Apply Gram’s iodine solution to the slide, covering the stained sample thoroughly.
- The iodine forms a complex with the crystal violet, enhancing its adhesion to the bacterial cell wall.
c. Decolorization:
- Gradually add the decolorizer (e.g., ethanol or acetone) to the slide, drop by drop.
- This step is critical and requires careful monitoring. Over-decolorization can lead to false-negative results for Gram-positive bacteria.
d. Counterstaining with Safranin:
- After decolorization, wash the slide with water to remove excess decolorizer.
- Apply safranin solution to the slide, covering the entire sample.
- Safranin serves as a counterstain, imparting a contrasting red color to Gram-negative bacteria.

3. Microscopic Examination:
- The slide should undergo examination under a microscope, initially using the X40 objective to evaluate the smear distribution. Then, examine them using the X100 oil immersion objective.
- All areas of the slide require an initial examination. Areas that are only one cell thick should be examined. Thick areas in slides often give variable and incorrect results.
- White blood cells and macrophages stain Gram-negative, while squamous epithelial cells stain Gram-positive.
Interpreting Results:
The interpretation of results is crucial for determining the presence and type of bacteria in the sample.
- Gram-Positive Bacteria: Retain the crystal violet dye, appearing purple or blue under the microscope.
- Gram-Negative Bacteria: Lose the crystal violet dye but are counterstained with safranin, appearing pink or red.

Interfering Factors in Gram Staining:
Gram staining, being a sensitive procedure, can be affected by several factors:
- Specimen Collection: Proper sterile collection is crucial to prevent contamination. Prior antibiotic use can hinder organism growth.
- Analysis under Low Power (10X):
- Background should appear gram-negative or clear.
- White blood cells should stain gram-negative; their gram-positive staining may indicate errors.
- Differentiating thin crystal violet from bacteria is crucial.
- Smears should be uniform and one cell thick without overlap.
- Low Power Examination:
- Note relative numbers of cells, such as leukocytes and epithelial cells.
- Observe bacterial arrangements and shapes for clues to identification.
- Oil Immersion (100X):
- Identify and document bacterial morphology, including shape, ends, sides, and axis.
- Note pleomorphism, branching, or extensions.
Adhering to these guidelines ensures accurate Gram stain interpretation, aiding in precise diagnosis and treatment of bacterial infections.
Clinical Significance:
Gram staining aids in the diagnosis of bacterial infections and guides treatment decisions by providing rapid preliminary results regarding the type of bacteria present.
Conclusion:
Gram staining remains an invaluable tool in microbiology, allowing for rapid and reliable differentiation of bacterial types. By understanding the principle, procedure, and interpretation of results, healthcare providers can make informed decisions regarding patient care and treatment strategies in cases of suspected bacterial infections.
References:
- Leopold JA, Ferraro MJ. (2020). Microbiology Concepts & Applications. McGraw-Hill Education.
- Forbes BA, Sahm DF, Weissfeld AS. (2007). Bailey & Scott’s Diagnostic Microbiology. Mosby Elsevier.
- Tortora GJ, Funke BR, Case CL. (2017). Microbiology: An Introduction. Pearson Education.
- Wilson B. (2017). Staining Procedures. In: Wilson B, editor. Techniques in Microbiology: A Student Handbook. Cengage Learning.
- American Society for Microbiology. (2005). Basic Protocol 1: Gram Staining of Bacterial Cultures. In: Walker JM, editor. The Protein Protocols Handbook. Humana Press.
Biochemical tests for identification of Gram negative bacteria (thesciencenotes.com)