Inappropriate immune responses can lead to tissue damage. When someone has been immunologically primed, re-exposure with antigen leads to secondary boosting of the immune response. The reaction is normally employed by the body in fighting infection. However, the reaction could also be excessive, leading to tissue damage. Such undesirable reaction produced is known as hypersensitivity and includes allergy and autoimmunity.
Allergy
Allergy is an immunological reaction of the body to external antigens – allergens.
Allergens
Allergens are substances usually protein in nature and exist normally within the environment. Simple low mass substances are only partial antigens (hapten), become a whole antigen within the body after binding with internal protein.
Autoimmunity
In contrast to allergy, is an immunological reaction in which the system directly or indirectly targets and damages its own cells. The effect may range from discomfort, organ damage, to fatality.
Classification of Hypersensitivity
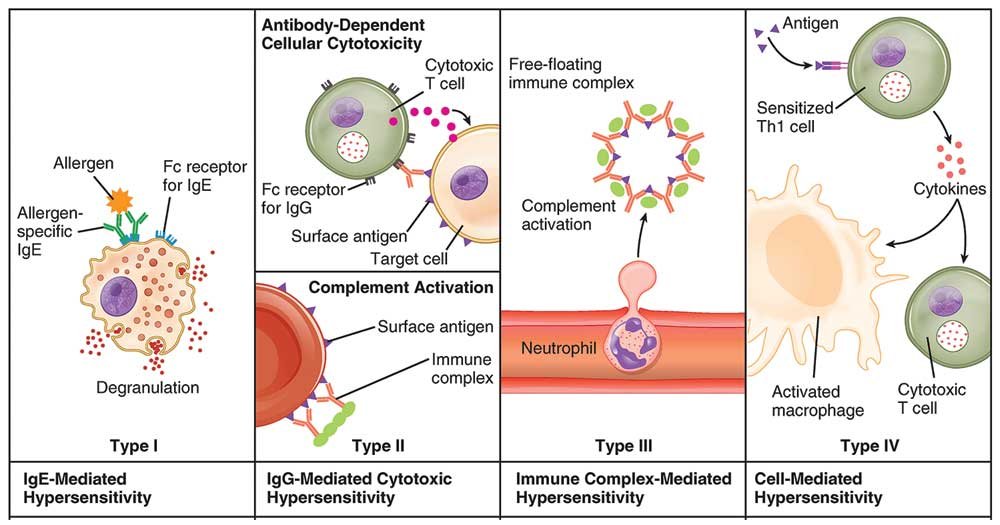
Until 1960s, systematic classification of hypersensitivity as well allergic diseases was difficult. Later in 1963, Coombs and Gell described a “classification of allergic reactions which may be deleterious to the tissues and harmful to the host” 1 . According to Gell and Coombs classification, hypersensitivity is of four different types: I, II, III and IV. Type I, II, and III are antibody-mediated whereas type IV is mediated by T cells.
Type I (Immediate Hypersensitivity)
Type I hypersensitivity is an allergic reaction provoked by re-exposure to a specific antigen called an allergen. IgE antibodies bind to receptors (FcεRI) found on the surface of tissue mast cells and blood basophils and sensitize them 2. Upon secondary exposure, the IgE on the surface of the sensitized mast and basophil cells becomes cross-linked. When two IgE receptors are cross-linked, signal transduces through the γ chains of the receptor leading to an influx of calcium, which initiates both degranulation and release of mediators such as histamines, leukotriene, and prostaglandin into the extracellular environment within minutes, producing allergic reactions. As the reaction occurs within a few minutes, type I hypersensitivity is also known as immediate hypersensitivity. Some examples are anaphylaxis, food allergies, drug allergies and dust allergies.
Type II (Antibody-Dependent Cytotoxic Hypersensitivity)
Type II hypersensitivity is mediated by antibodies, IgG and IgM. The antibodies are directed against the antigen (self or non-self) on cells of particular tissue and hypersensitivity occurs by the following mechanisms:
a) Attack by antibodies activates the complement cascade causing target cell destruction. b) Antibody-dependent cellular cytotoxicity (ADCC) may be exhibited by both non-phagocytic natural killer (NK) cells or by phagocytic cells, such as polymorphs and monocytes. Some examples are autoimmune hemolytic anemia, pernicious anemia, transfusion reactions (Rh incompatibility) and rheumatic fever.
Type III (Immune Complex-Mediated Hypersensitivity)
In type II hypersensitivity, IgG binds to the free antigens and immune complexes are formed. The immune complexes thus formed, circulate in the free state and under circumstances of increased vascular permeability, deposits at certain tissues such as: a) Blood vessel walls (vasculitis) b) Synovial joints (arthritis) c) Glomerular basement membrane (glomerulonephritis) The deposition of immune complexes results in the activation of the complement system and chemotaxis of polymorphs to the site of immune complex deposition causing local tissue damage and inflammation 3. Some more examples are serum sickness, systemic lupus erythematosus (SLE), and post-streptococcal glomerulonephritis.
Type IV (Delayed-Type Hypersensitivity)
Type IV hypersensitivity is additionally called delayed-type hypersensitivity as the reaction takes several days to develop. It is mediated by T-cells and is antibody independent 4. Robert Koch was first to discover the reaction in 1882 but, only in 1940s it was proved that the reaction is mediated by the cellular and not the humoral arm of the immune system by Landsteiner and Chase5.
The delayed-type hypersensitivity reaction involves two phases:
a) Sensitization phase: The primary exposure to antigens sensitizes T-memory cells (major player TH1 cells). Sensitizing agents for humans include metal ions, like nickel and chromium, various industrial chemicals and natural products present in dyes, drugs, fragrances, and plants.
b) Effector phase: Upon secondary exposure of pre-sensitized TH1 with the same antigen, the stimulated T-cells release a number of pro-inflammatory cytokines and chemokines. The released mediators attract and activate macrophages and cytotoxic T-cells leading to inflammation and tissue damage. Some examples are multiple sclerosis, contact dermatitis, and type-I diabetes mellitus.
References
1. Kay AB, Kaplan AP, Bousquet J, Holt PG, Kay AB. Immunology of the Allergic Response 1 Allergy and Hypersensitivity: History and Concepts. Allergy Allerg Dis. 2008:1-22. http://login.research4life.org/tacsgr1onlinelibrary_wiley_com/doi/p df/10.1002/9781444300918.ch1.
2. Justiz Vaillant AA, Zito PM. Hypersensitivity Reactions, Immediate.; 2018.
3. Rajan T V. The Gell–Coombs classification of hypersensitivity reactions: a re-interpretation. Trends Immunol. 2003;24(7):376-379. doi:10.1016/S1471-4906(03)00142-X
4. Warrington R, Watson W, Kim HL, Antonetti FR. An introduction to immunology and immunopathology. Allergy, Asthma Clin Immunol. 2011;7(S1):S1. doi:10.1186/1710-1492-7-s1-s1
5. Black CA. Delayed type hypersensitivity: current theories with an historic perspective. Dermatol Online J. 1999;5(1):7.