Hypersensitivity reactions, intricate immune responses that can cause harm, fall into categories based on onset and mechanisms. Immediate hypersensitivity, known as type I hypersensitivity, stands out. This reaction involves chemical mediators released from mast cells and basophils, setting off a series of events that lead to diverse allergic symptoms. In this detailed article, we delve into the workings of hypersensitivity type I, its clinical presentations, and available treatments.
Type I Hypersensitivity Reaction: A Quick Overview
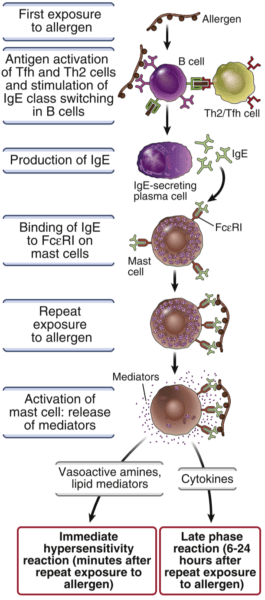
Type I hypersensitivity, or immediate hypersensitivity, is marked by IgE-mediated responses. This reaction happens rapidly, within minutes of allergen exposure, releasing chemical mediators causing allergic symptoms. The process starts with sensitization, where IgE antibodies form in response to allergens. These antibodies attach to mast cells and basophils, priming them for future reactions.
Upon reexposure to the allergen, it binds to IgE antibodies on mast cells and basophils, triggering degranulation. This leads to changes in affected tissues, resulting in symptoms like swelling, itching, and bronchoconstriction.
Essential Components of Hypersensitivity Type I
Allergens:
Allergens, inciters of amplified immune responses, provoke IgE-mediated reactions on repeated exposure in allergic individuals. Notably, allergens differ in potency. Strong antigens include foreign serum and egg albumin, while pollen is a milder antigen. Common allergens encompass foreign serum, vaccines, plant pollens like ryegrass and ragweed, drugs like penicillin and sulfonamides, foods including nuts and seafood, insect products like bee venom and dust mites, mold spores, and animal hair and dander.
IgE:
IgE, an antibody, is typically secreted minimally. However, during parasitic infections, its secretion increases to fight parasites. Atopy refers to a genetic tendency allowing non-parasitic antigens to stimulate excessive IgE production, causing tissue-damaging type I hypersensitivity reactions. Atopic individuals can produce up to ten times more IgE than normal. TH1 cells, with interferon-gamma, suppress IgE production. IgE, or reagin, plays a role in allergic reactions and serves as a cytotoxic antibody.
Mast Cells and Basophils:
Basophils, granulocytes circulating in the bloodstream, move to inflammation sites. Mast cells, located in connective tissue near vessels, nerves, and mucous membranes, house active mediators. Activation leads to granule release, sparking type I hypersensitivity reactions.
IgE Binding Fc Receptor:
IgE’s reaginic activity hinges on binding to Fc receptors on mast cells and basophils, with high- and low-affinity receptors present.
Mediators and Cytokines:
Clinical symptoms of type I reactions arise from mediator release during mast cell and basophil degranulation. These mediators affect local tissues and effector cells like eosinophils, neutrophils, monocytes, T lymphocytes, and platelets. While helpful against parasites, allergen-induced responses lead to damaging inflammation and increased vascular permeability.
Mediator Classification:
Mediators fall into primary or secondary categories. Primary mediators, pre-formed and stored in granules, precede degranulation. Secondary mediators are either synthesized after target cell activation or released via cell membrane breakdown during degranulation.
Understanding the elements of hypersensitivity type I deepens insight into allergic reactions. Allergens, IgE, mast cells, basophils, and mediators play vital roles in initiating and sustaining these reactions.
Steps of Hypersensitivity Type I
Hypersensitivity Type I, immediate hypersensitivity or allergic hypersensitivity, comprises multiple elements and stages in its process. Triggered by interaction between specific allergens and IgE antibodies, this reaction releases various chemical mediators from mast cells and basophils. Dive into Hypersensitivity Type I components:
Allergen (Antigen):
Allergen exposure starts the process. Allergens come from diverse sources, including pollen, dust mites, foods, and medications.
| Allergen Type | Examples |
| Proteins | Foreign serum, vaccines |
| Plant Pollens | Ryegrass, ragweed, birch trees, timothy grass |
| Drugs | Penicillin, sulfonamides, local anesthetics |
| Foods | Nuts, seafood, eggs, milk, soy, wheat |
| Insect Products | Bee venom, wasp venom, mosquito bites |
| Animal Allergens | Pet dander (cats, dogs), animal saliva, urine |
| Mold Spores | Alternaria, Aspergillus, Cladosporium |
| Dust Mites | Dermatophagoides pteronyssinus, Dermatophagoides farinae |
| Latex | Latex gloves, medical equipment |
| Cockroach Allergens | Cockroach feces, saliva, body parts |
- Sensitization: Initial exposure triggers an immune response. Antigen-presenting cells (APCs) process allergens, presenting them to helper T cells (Th2 cells). Th2 cells then secrete interleukin-4 (IL-4) and interleukin-13 (IL-13).
- B Cell Activation and IgE Production: IL-4 and IL-13 prompt B cell differentiation into plasma cells producing IgE antibodies. These antibodies attach to the Fcε receptors on mast cells and basophils.
- IgE Binding to Mast Cells and Basophils: Circulating IgE antibodies bind to receptors on mast cells (connective tissue) and basophils (bloodstream). These cells are found in skin, respiratory, and gastrointestinal areas.
- Sensitized Mast Cells and Basophils: IgE binding sensitizes these cells to the allergen. This readies them for a swift and heightened immune response upon allergen reexposure.
- Reexposure and Degranulation: Allergen binding to IgE antibodies triggers degranulation via cross-linking, releasing stored mediators.
- Degranulation and Mediator Release: Stored mediators like histamine, leukotrienes, prostaglandins, and cytokines are released, contributing to symptoms.
- Clinical Manifestations: Released mediators cause distinct clinical signs. These range from skin reactions like hives and itching to respiratory symptoms like sneezing and coughing, gastrointestinal distress, and severe systemic anaphylaxis requiring immediate medical intervention.
Reactions of Immediate Hypersensitivity: Immediate and Late Phase Reaction
Immediate hypersensitivity, also known as Type I hypersensitivity, involves two distinct phases of allergic reactions: the immediate phase and the late phase. These reactions occur rapidly after exposure to allergens and are mediated by immune mechanisms involving IgE antibodies, mast cells, and other immune cells. Here’s an overview of both phases:
Immediate Phase Reaction:
- Onset: Occurs within minutes of allergen exposure.
- Mechanism: Upon initial exposure to an allergen, IgE antibodies are produced and attach to mast cells and basophils.
- Reexposure: When the same allergen is encountered again, it binds to the IgE antibodies on mast cells and basophils.
- Degranulation: Cross-linking of IgE antibodies triggers the release of pre-formed mediators (histamine, proteases, heparin, etc.) stored in mast cell granules.
- Clinical Manifestations: Rapid onset of symptoms, including itching, redness, hives, swelling (angioedema), sneezing, runny nose, coughing, wheezing, shortness of breath, and in severe cases, systemic anaphylaxis.
Late Phase Reaction:
- Onset: Develops hours after the immediate phase (usually 4 to 6 hours).
- Mechanism: Involves recruitment of inflammatory cells, such as eosinophils and neutrophils, to the site of allergen exposure.
- Cellular Response: Activation of Th2 lymphocytes leads to the release of cytokines, attracting immune cells to the site and amplifying inflammation.
- Clinical Manifestations: Symptoms include prolonged redness and swelling at the site of allergen exposure, increased mucus production, persistent cough, and ongoing airway constriction.
- Associated Conditions: Late-phase reactions are often seen in chronic allergic conditions like allergic asthma.
Key Differences:
- The immediate phase is characterized by rapid release of pre-formed mediators from mast cells, causing acute symptoms.
- The late phase involves a delayed inflammatory response with recruitment of immune cells and cytokine release, leading to prolonged and lingering symptoms.
Roles of Mast Cells and Basophils
Mast cells and basophils play central roles in type I hypersensitivity. When sensitized by IgE antibodies, they release stored and newly synthesized mediators upon allergen engagement. These mediators drive allergic responses in various tissues, manifesting as symptoms.
Diagnosis and Treatment
Diagnosing type I hypersensitivity involves clinical history, examination, and allergy testing. Tests like skin prick tests or IgE level measurements in blood identify triggering allergens. Proper diagnosis involves thorough patient history and skin tests showing responses to allergens, aiding in identifying the cause. Treating type I hypersensitivity focuses on symptom management and preventing severe reactions. For acute anaphylaxis, prompt self-injection of epinephrine is crucial. Medications like antihistamines and bronchodilators help, with immunotherapy as a longer-term solution.
Conclusion
Hypersensitivity type I, immediate hypersensitivity, involves IgE-mediated responses, mast cells, and basophils. This spectrum spans mild discomfort to life-threatening anaphylaxis. Understanding mechanisms and clinical manifestations empowers patients and healthcare professionals to manage and treat allergic conditions. Proper diagnosis, avoidance strategies, and tailored treatments enhance the quality of life for those with type I hypersensitivity.
References
- Galli, S. J., & Tsai, M. (2012). IgE and mast cells in allergic disease. Nature Medicine, 18(5), 693-704.
- Pawankar, R., Canonica, G. W., Holgate, S. T., & Lockey, R. F. (Eds.). (2014). Allergic diseases: Mechanisms and treatment. John Wiley & Sons.
- Plaut, M., Valentine, M., Longbottom, J. L., & Schulman, E. S. (1991). Studies of IgE-dependent histamine-releasing factors: evidence for a role in allergen-induced bronchoconstriction. Journal of Immunology, 147(5), 1640-1647.
- Sampson, H. A., Muñoz-Furlong, A., & Campbell, R. L. (2006). Second symposium on the definition and management of anaphylaxis: summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Journal of Allergy and Clinical Immunology, 117(2), 391-397.
- Galli, S. J., & Tsai, M. (2010). Mast cells: versatile regulators of inflammation, tissue remodeling, host defense and homeostasis. Journal of Dermatological Science, 49(1), 7-19.
- Akdis, C. A., Akdis, M., Blesken, T., Wymann, D., Alkan, S. S., Müller, U., & Blaser, K. (1998). Epitope-specific T cell tolerance to phospholipase A2 in bee venom immunotherapy and recovery by IL-2 and IL-15 in vitro. Journal of Clinical Investigation, 102(4), 716-722.
- Boyce, J. A. (2019). Mast cells and eosinophils in allergic inflammation. Frontiers in Immunology, 10, 1461.
- Gould, H. J., Sutton, B. J., & Beavil, A. J. (2003). The biology of IGE and the basis of allergic disease. Annual Review of Immunology, 21(1), 579-628.
Learn more