Nipah virus (NiV) is a zoonotic virus that may infect both humans and animals and cause serious sickness. During an outbreak in Malaysia and Singapore in 1998, it was initially discovered. The name of the virus comes from the Malaysian the village of Sungai Nipah.
It primarily originates from fruit bats, also known as flying foxes. However, Other animals, such as pigs, goats, horses, dogs, and cats, can also spread the infection.
Nipah virus (NiV) transmission
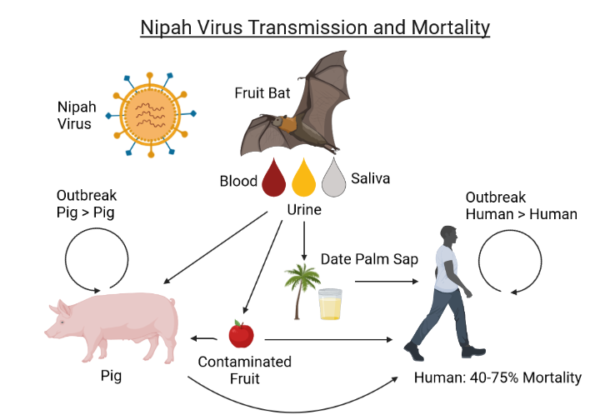
The Nipah virus (NiV) transmission can occur through various means, with the primary mode of transmission being from animals, particularly bats, to humans. Here are the various means of transmission:
Direct contact with infected animal:
When people or animals come into contact with an infected animal’s bodily fluids (blood, feces, urine, or saliva), transmission takes place.
Food Products contaminated by Infected Animals:
Eating food products that have been contaminated by an infected animal can potentially make us sick. Raw date palm fruit or sap should be used with particular care.
Person-to-Person NiV is infectious and can be passed from person to person by bodily fluids. As a result, being in close contact to an infected person poses a risk, particularly when providing care.
Where is Nipah virus found?
The Nipah virus is mostly present in South and Southeast Asia, while rare cases have been noted in a few places. In 1999, the virus was initially identified after it caused 100 deaths in Malaysia and Singapore. The infection caused the death of almost 1 million pigs, which had a significant negative economic effect on countries around the world. There have been approximately 20 more outbreaks since 1999.
Fruit bats, especially members of the Pteropodidae family, serve as its natural reservoir host. The virus is carried by these bats, which are frequently seen in these areas and do not show any signs of sickness. Countries including Malaysia, Singapore, Bangladesh, and India have all been linked to the Nipah virus. In places where people, animals, especially pigs, and fruit bats contact often, outbreaks frequently happen. In communities and agricultural settings with high concentrations of these intermediate hosts, there have been occurrences of Nipah virus infection in humans.
Symptoms and causes of Nipah virus
Nipah virus infection can cause a range of symptoms, which can vary in severity. The incubation period for is typically 5 to 14 days after exposure, and symptoms may include:
- Fever: A sudden, high fever is a common symptom of the Nipah virus infection.
- Headache: A common early sign of virus infection is headaches.
- Muscle pain: The infections can cause generalized muscle pain in affected individuals.
- Fatigue: Extreme fatigue and weakness are common signs.
- Respiratory symptoms, such as a cough, sore throat, and breathing difficulties, may occasionally occur.
- Vomiting and nausea: Vomiting and nausea might happen, frequently resulting in dehydration.
- Neurological symptoms include dizziness, disorientation, and altered awareness. As the infection gets worse, the central nervous system may also be affected.
- Seizures: In more serious cases of virus infection, seizures may happen.
- Encephalitis: Nipah virus is known for causing encephalitis, which is inflammation of the brain. This can result in confusion, hallucinations, and coma.
- Mental Confusion: People who have the virus infection may have memory loss, personality abnormalities, and mental dizziness.
- Coma: In severe situations, the infection may spread quickly and result in a potentially fatal coma.
It’s essential to understand that the severity of a Nipah virus infection can vary, with some people showing milder symptoms and others continuing to have more serious and perhaps fatal sickness. In some pandemics, the patient fatality rate for virus infection can range from 40% to 75%. Strict infection control measures are necessary to limit its spread and early diagnosis and treatment are critical for increasing the probability of survival.
How is Nipah virus is diagnosed?
Nipah virus (NiV) infection is diagnosed using a combination of clinical assessment, laboratory testing, and epidemiological research. For proper medical treatment and the implementation of steps to stop the virus’s spread, early detection is essential. The main Nipah virus diagnostic techniques and assays are listed below:
Clinical Assessment:
Medical experts evaluate a patient’s symptoms, medical background, and suspected Nipah virus exposure. Important clinical signs include a high fever, neurological symptoms, and a history of contact with sick people or animals in outbreak areas.
Blood and Serum Tests:
From suspected cases, blood and serum samples are taken and sent to specialized labs for analysis. Common tests consist of:
- Reverse Transcription Polymerase Chain Reaction (RT-PCR): This molecular test detects the virus’s genetic material (RNA) in serum or blood. It is an extremely sensitive and accurate method to diagnose Nipah virus infection.
- ELISA, or enzyme-linked immunosorbent assay, is a test that may identify IgM and IgG antibodies to the virus in blood. IgG antibodies often emerge later in the illness, whereas IgM antibodies are typically present early on. ELISA is useful in establishing previous viral exposure.
Lumbar puncture may be used to collect cerebrospinal fluid (CSF) for investigation in cases of encephalitis or neurological symptoms. Sometimes viral RNA can be found in CSF, indicating that the central nervous system has been affected.
Virus Isolation: Virus isolation from clinical samples, such as blood or saliva samples, can give definitive proof of virus infection. Due to the risk of contracting a live virus, virus isolation is normally done in high-containment labs.
Histopathology: In some instances, tissues from deceased people may be examined post-mortem and show distinctive histopathological changes consistent with Nipah virus infection.
Serological Surveys: To assess the level of viral exposure during outbreak investigations, serological surveys may be carried out among residents of the affected communities.
Prevention of Nipah virus
- Avoid contact with Bats.
- Practice good hygiene.
- Limit consumption of date palm sap.
- Avoid close contact with sick individual.
- Use personal protective equipment (PPE).
- Practice safe animals handling.
- Quarantine and cull infected animals.
- Vaccination and antiviral research.
Learn more about
References
- https://my.clevelandclinic.org/health/diseases/25085-nipa-virus
- https://www.lumahealth.com/understanding-nipa-virus-risks-symptoms-prevention/
- https://www.cdc.gov/vhf/nipa/prevention/index.html
- https://www.osmosis.org/answers/nipa-virus