History and Development
Penicillin, derived from the Penicillium fungi, is a group of antibiotics that revolutionized medicine. Its discovery is credited to Scottish microbiologist Alexander Fleming, who observed in 1928 that a mold had contaminated his petri dish and eradicated the bacteria he had been studying, leading to the development of one of the most widely used antibiotics in history.
Following this discovery, researchers Howard Florey and Ernst Chain from the University of Oxford worked to isolate and produce the antibiotic in large quantities. In 1941, they successfully treated their first patient, Albert Alexander, a policeman who had a severe infection that had spread to his eyes, scalp, and lungs. Alexander’s recovery marked a significant breakthrough in medicine, paving the way for mass production.
During World War II, penicillin played a vital role in treating injured soldiers, saving millions of lives. By the 1950s, it became widely available to the public, continuing its dominance in the battle against bacterial infections.
Despite its widespread use today, it has become less effective against some bacteria strains due to the emergence of antibiotic resistance. Nevertheless, the discovery of penicillin remains a crucial milestone in medical history, and its contributions to fighting infections are immeasurable.
Structure of Penicillin
Penicillin is a widely used antibiotic that belongs to the beta-lactam family of antibiotics. Its unique structure is crucial for its ability to kill bacteria, and understanding this structure is essential for the development of new and more effective antibiotics.
Here are the key points about the structure:
Penicillin contains a beta-lactam ring and a thiazolidine ring.
- The beta-lactam ring is a four-membered cyclic amide, which is essential for the antibiotic’s antimicrobial activity. The ring mimics the bacterial cell wall precursors, such as peptidoglycan, inhibiting bacterial cell wall synthesis.
- The thiazolidine ring contributes to the antibiotic’s pharmacological properties and enhances its efficacy against gram-positive bacteria. It is also responsible for the stability of the beta-lactam ring and the resistance of penicillin to acid degradation.
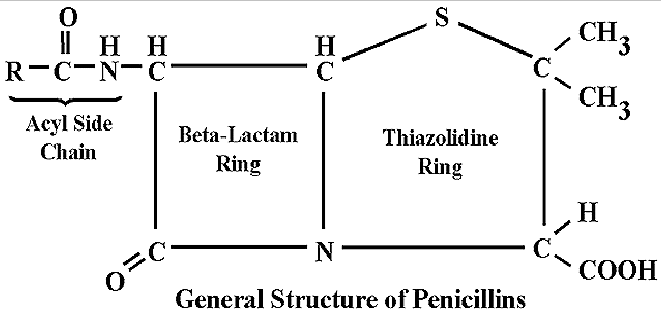
- The specific structure can vary depending on the type of penicillin, with different side chains attached to the beta-lactam ring. This variability allows for the development of different forms with varying spectra of activity and resistance patterns.
- The beta-lactam ring is also responsible for the development of resistance to penicillin. Bacteria produce enzymes called beta-lactamases, which can break the beta-lactam ring, rendering the antibiotic ineffective.
Mechanism of Action of Penicillin
Penicillin is a widely used bactericidal antibiotic that works by inhibiting bacterial cell wall synthesis. Here are the key points about its mechanism of action:
- Penicillin binds to and inhibits transpeptidases, which are responsible for cross-linking the peptidoglycan strands in bacterial cell walls.
- The beta-lactam ring is essential for its mechanism of action as it is structurally similar to the D-Ala-D-Ala portion of the peptidoglycan precursors, allowing it to bind to transpeptidases.
- By inhibiting transpeptidases, penicillin prevents the formation of new peptidoglycan cross-links, resulting in weakened cell walls that are unable to withstand the osmotic pressure of the bacterial cell. This leads to cell lysis and death.

- Penicillin is most effective against actively growing bacterial cells that are synthesizing new peptidoglycan. Bacteria in stationary phase or those with inactive transpeptidases may be less susceptible to it.
- The spectrum of activity of penicillin is limited to gram-positive bacteria and some gram-negative bacteria such as Neisseria and Haemophilus, as gram-negative bacteria have an outer membrane that prevents antibiotic from reaching the peptidoglycan layer of the cell wall.
- The use of penicillin can lead to the development of antibiotic resistance, as bacteria can produce enzymes called beta-lactamases that break down the beta-lactam ring of penicillin, making it ineffective. Bacteria can also modify their cell wall structure to make it less susceptible to antibiotic.
Penicillin inhibits bacterial cell wall synthesis through binding to transpeptidases and preventing the formation of new peptidoglycan cross-links. Its mechanism of action is dependent on the beta-lactam ring, and it is most effective against actively growing gram-positive bacteria. However, the use of penicillin can lead to the development of antibiotic resistance, making it less effective against certain bacteria.
Antimicrobial Activity of Penicillin
Penicillin is a powerful antibiotic that can effectively combat a range of bacterial species, particularly gram-positive bacteria like Streptococcus, Staphylococcus, and Clostridium that have a thick peptidoglycan layer in their cell walls.
Penicillin’s mechanism of action involves binding to transpeptidases and preventing the formation of new peptidoglycan cross-links, thereby inhibiting bacterial cell wall synthesis and ultimately leading to cell lysis and death.
Although primarily effective against gram-positive bacteria, penicillin can also be active against some gram-negative bacteria like Neisseria and Haemophilus. However, the outer membrane of gram-negative bacteria can make it difficult for antibiotic to penetrate and reach the peptidoglycan layer of their cell wall.
Penicillin is not effective against all types of bacteria, including anaerobic bacteria like Bacteroidesand some gram-negative bacteria like Pseudomonas aeruginosa.
Overuse and misuse of antibiotics can lead to the emergence of antibiotic-resistant strains of bacteria, making it more challenging to treat bacterial infections. Bacteria can produce enzymes called beta-lactamases that break down the beta-lactam ring of penicillin, rendering it ineffective. They can also modify their cell wall structure to make it less susceptible to penicillin.
In conclusion, while penicillin is a potent antibiotic with broad-spectrum activity against many bacterial species, the emergence of antibiotic-resistant strains of bacteria highlights the need for cautious and judicious use of antibiotics to preserve their effectiveness in treating bacterial infections.
Antibiotic resistance mechanism against Penicillin
Bacteria can develop antibiotic resistance through various mechanisms.
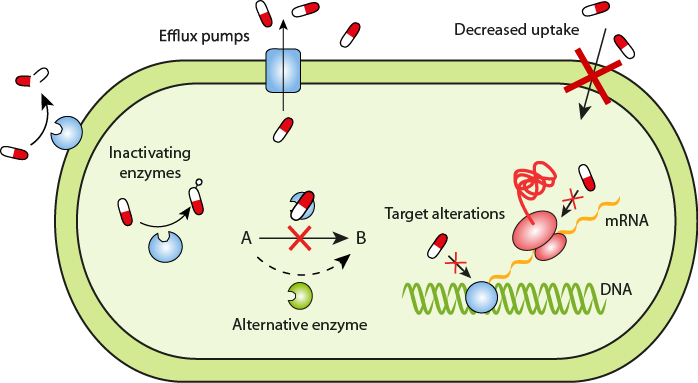
- One of the main mechanisms of resistance is the production of beta-lactamase enzymes that break down the beta-lactam ring of penicillin, rendering it ineffective.
- Some bacteria can also develop resistance by modifying their cell wall structure, making it less susceptible to the effects of penicillin.
- Another mechanism of resistance is the overexpression of efflux pumps, which can actively remove the antibiotic from the bacterial cell before it can exert its effects.
- Bacteria can also acquire resistance genes from other bacteria through horizontal gene transfer, leading to the spread of antibiotic resistance.
- Overuse and misuse of antibiotics have contributed to the emergence of antibiotic-resistant strains of bacteria, making the treatment of bacterial infections more challenging.
Classification of Penicillin
Penicillins are a crucial group of antibiotics used to fight bacterial infections. These antibiotics are classified based on their spectrum of activity and chemical structure. There are four primary types of penicillins, including natural penicillins, aminopenicillins, extended-spectrum penicillins, and beta-lactamase inhibitors.
1. Natural penicillins
Natural penicillins are the original form and are produced by the Penicillium fungus. They have a narrow spectrum of activity and are effective against Gram-positive bacteria. Examples include penicillin G, penicillin V, and benzylpenicillin.
2. Aminopenicillins
Aminopenicillins are a broad-spectrum type of penicillin that can effectively combat both Gram-positive and Gram-negative bacteria. They are more potent than natural penicillins and include ampicillin and amoxicillin.
3. Extended-spectrum penicillins
Extended-spectrum penicillins have an even broader spectrum of activity and can combat bacteria that are resistant to other types. They include piperacillin and ticarcillin.
4. Beta-lactamase inhibitors
Beta-lactamase inhibitors are not penicillins themselves but are combined with them to prevent the breakdown of the antibiotic by beta-lactamase enzymes produced by some bacteria. Some examples of beta-lactamase inhibitors include clavulanic acid, sulbactam, and tazobactam.

Aside from these four primary types, there are also other variations that have been developed, such as antistaphylococcal penicillins, which are effective against Staphylococcus aureus bacteria, and carbapenems, which are a type of beta-lactam antibiotic often used as a last resort for severe infections.
Adverse Effects of Penicillin
Penicillin is generally well-tolerated, but like all medications, it can cause adverse effects in some people.
- The most common adverse effects gastrointestinal in nature, such as nausea, vomiting, and diarrhea.
- Allergic reactions are also possible, ranging from mild skin rashes to severe anaphylaxis.
- Anaphylaxis is a severe, potentially life-threatening allergic reaction that can cause difficulty breathing, low blood pressure, and shock.
- People who have a history of allergic reactions to penicillin or other beta-lactam antibiotics should not take the antibiotic unless they are under close medical supervision.
- Other rare adverse effects of penicillin include kidney damage, blood disorders, and seizures.
- Long-term use of antibiotic can also disrupt the normal balance of bacterial flora in the body, leading to overgrowth of resistant bacteria and other complications.
If you experience any adverse effects while taking penicillin, you should contact your healthcare provider immediately. They may need to adjust your dosage or switch you to a different antibiotic.