Abruptio placentae is defined as bleeding from or into the genital tract that occurs after the 28th week of pregnancy but before the birth due to premature separation of normally situated placenta. It is also termed as accidental hemorrhage, premature separation of placenta. In about 1 in 200 pregnancies, abruption placentae are seen.
Who are at risk of developing placental abruption?
- Previous history of placental abruption: Recurrence 5-17%
- Pregnancy with gravid more than or equals to 5 are at high risk
- Increased maternal age
- Hypertension in pregnancy: 10-50% are at risk of developing placenta previa
- Trauma
- Cigarette smoking
- Cocaine abuse
- Sudden uterine decompression usually seen following delivery of first baby of twins, polyhdramnios due to sudden escape of liquor, premature rupture of membrane.
- Placental abruption are also seen in cases with short cord, supine hypotension syndrome, placental anomalies, folic acid deficiency, thrombophilias
Types of Abruptio Placenta
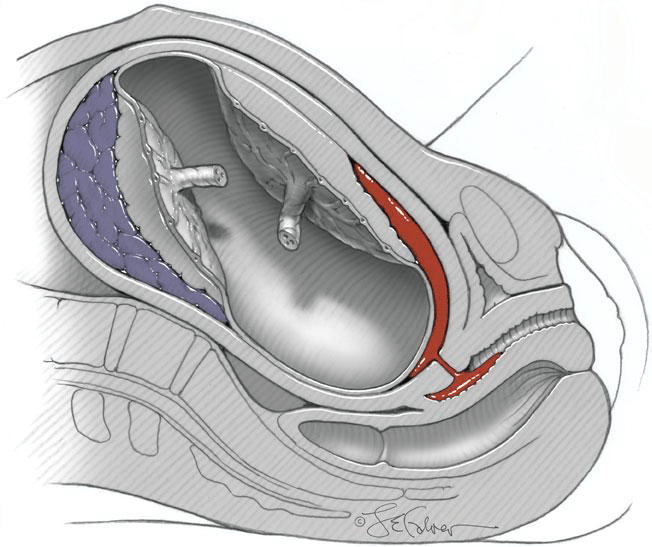
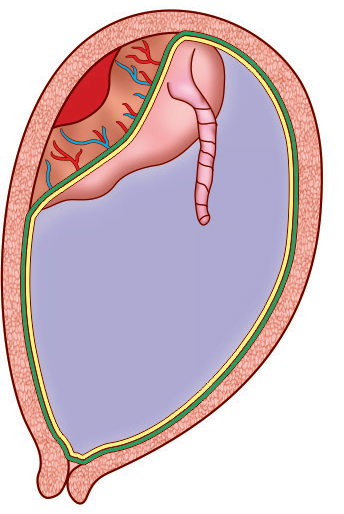
Revealed type Abruptio Placenta
In this variety bleeding is usually visible coming out of cervical canal and is one of most common type.
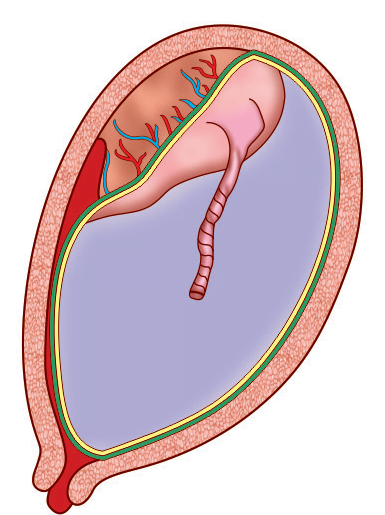
Concealed type abruptio placentae
In this variety blood usually collects in between membranes and decidua and blood is prevented coming out of cervix.
Mixed Type Abruptio placenta
In this variety combination of revealed and concealed are seen and usually one variety predominates over other.
What are the changes seen in different organs?
- Dark port wine color uterus which may be patchy or diffuse is seen.
- Retroplacental hematoma is usually seen after expulsion of placenta.
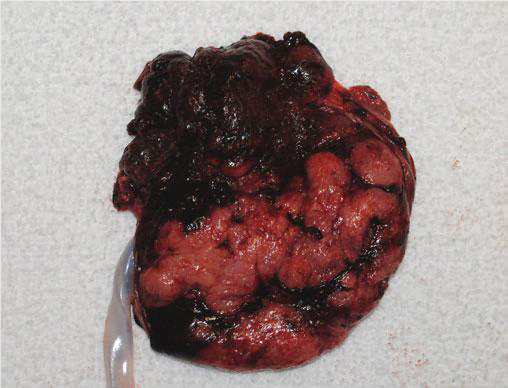
- In some cases, there is an intravasation of blood occurs in the musculature of uterus upto serous coat and termed as couvelaire uterus. It can only be diagnosed on laparotomy.
- There is presence of fibrin knots in hepatic sinusoids.
- In kidney acute tubular necrosis is seen.
- Shock proteinuria is seen.
How does patient with abruptio placentae presents?
Symptoms of abruptio placentae
- Abdominal pain which is severe and constant and is more in concealed than revealed type.
- Bleeding is seen in revealed and mixed type and usually preceeded by trauma.
- Bleeding is not recurrent and there is no warning hemorrhage.
Signs of abruptio placentae
- General condition may be out of proportion to extent of bleeding in concealed type.
- Hypertension may be present.
- Size of uterus will be more than expected size according to period of gestation and may be tense, tender, even rigid.
- Fetal distress or even fetal death.
Clinical classification of Abruptio placentae
Classification of abruptio placentae:
| Grade 0 | Grade 1 | Grade 2 | Grade 3 |
| Clinical features are usually absent | Slight vaginal bleeding | Mild to moderate vaginal bleeding | Mild to moderate vaginal bleeding |
| Diagnosed only after inspection of placenta following delivery. | Irritable uterus with minimal or absent uterine tenderness | Uterus is tender | Marked uterine tenderness |
| Good fetal heart sound | Fetal distress or even fetal death | Fetal death is always seen | |
| Maternal blood pressure and fibrinogen level is normal | Pulse rate is increased, blood pressure is maintained and decreased fibrinogen level | Shock is present and may be associated with coagulation defect or anuria |
What are other condition that is confused with abruption placenta?
- Placenta previa in case of revealed variety
- Mixed or concealed: Rupture uterus, rectus sheath hematoma, intestinal perforation, acute hydramnios, tonic uterine contraction
Investigations:
- Blood test: Complete blood count, hemoglobin, coagulation profile, blood grouping and cross matching, liver function test, urea and electrolyte.
- Ultrasonography: Hyperechoic or isoechoic is seen in early hemorrhage. Also fetal viability is assessed.
- Cardiotocography is done once mother is stable. It is usually helpful for timing and mode of delivery.
What are the complications seen in this case?
| Maternal | Fetal | ||
| Revealed | Concealed | Revealed | Concealed |
| Risk is proportional to visible blood loss Maternal death is rare | Hemorrhage Shock Blood coagulation disorder Oliguria and anuria Postpartum hemorrhage Puerperal sepsis | Fetal death | Fetal death due to prematurity and anoxia |
How can we manage Abruptio Placentae?
Preventive measures:
Primary prevention:
- Trauma is avoided.
- Sudden decompression of uterus should be avoided.
- Advice patient to lie in left lateral position to avoid supine hypotension.
- Routine administration of folic acid.
Secondary prevention:
- Early diagnosis and effective treatment.
Treatment in hospital
- Assessment of patient about: amount of blood loss, whether fetus is matured or not, patient is in labor or not, whether there is any complication or not, what is the type and grade of abruption placentae.
- Emergency management:
- Blood test: Hemoglobin and hematocrit estimation, blood grouping and cross matching, coagulation profile, Protrin in urine.
- Ringer’s lactate solution drip through wide bore iv cannula and arrangement of blood for transfusion if required.
- Monitor maternal and fetal condition.
- Immediate delivery is the definitive treatment.
- Revealed type:
- If patient is in labor, artificial rupture of membrane with or without oxytocin and vaginal delivery is done.
- If patient is not in labor, labor is induced with artificial rupture of membrane with or without oxytocin and vaginal delivery is done. If vaginal delivery is contraindicated, cesarean section is done.
- Concealed type:
- Artificial rupture of membrane with or without oxytocin, and vaginal delivery is done. If vaginal delivery is contraindicated cesarean section is done.
- Oxytocics should be continued to improve uterine tone with blood transfusion.
- Vaginal delivery can be performed in cases with:
- Limited placental abruption
- Reassuring fetal status
- If vaginal delivery can be performed soon
- Dead fetus
- Indications of cesarean section:
- Live fetus with severe placental abruption
- If cervix is unfavorable
- Bleeding is continuous even after amniotomy
- Fetal distress, oliguria and fibrinogen level is decreasing
References:
- DC Dutta’s Textbook of OBSTETRICS, 9th Edition
- Williams Obstetrics 24th Edition
- https://www.ajog.org/article/S0002-9378(15)00602-X/abstract
- https://pubmed.ncbi.nlm.nih.gov/17636217/