CD4 T Lymphocyte Cells, CD4+ T cells, also known as Helper T cells, are a subset of lymphocytes that aid in directing the immune response to infection and illness. They interact with one another and stimulate immune system cells such as macrophages, B lymphocytes (B cells), and CD8 T lymphocytes (CD8 cells), to fight infection.
CD4 T cells are referred to as “helper” cells since they stimulate the body’s response to infections rather than neutralizing viruses.
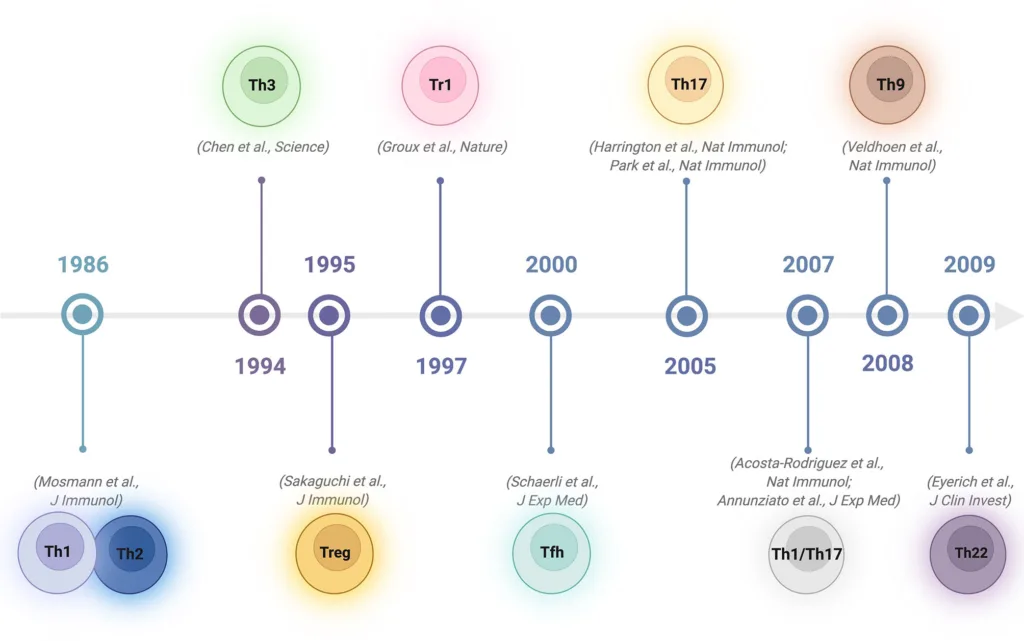
Naive CD4 T cells can develop into a variety of specialized subsets after being activated, each of which can generate a particular cytokine to support a distinct sort of immune response. After interacting with the antigen-MHC complex, they become activated and differentiate.
In addition to the conventional T-helper 1 (Th1) and T-helper 2 (Th2) cells, CD4+ cells can also develop into other subsets of cells. They include regulatory type 1 cells (Tr1), T-helper 17 (Th17), follicular helper T cells (Tfh), induced T-regulatory cells (iTreg), and the potentially unique T-helper 9 cells (Th9).
Source: https://www.frontiersin.org/articles/10.3389/fimmu.2022.867189/full
CD4 T Lymphocyte Cells Activation and Differentiation
The interaction of the TCR and CD4 as a co-receptor with the antigen-MHC II complex, which is presented by specialized antigen presentation cells (APCs), causes the antigenic stimulation that triggers the first stage of differentiation of the naive cells.
Naive cell proliferation and differentiation into particular effector cells are ultimately brought on by a network of downstream signaling pathways that are activated by the TCR in conjunction with CD3 activation.
Lineage-specific differentiation is influenced by the microenvironment’s cytokine milieu, Transcription factors, antigen concentration, APC type, and costimulatory molecule levels.
Function of CD4 T Lymphocyte Cells
While they are not directly involved in the neutralization of foreign chemicals, CD4+ T cells perform a number of other tasks that contribute to a strong immune response. They have different subsets, but they mostly stimulate other immune cells.
Activated CD4+ T cells have the capacity to develop into memory T cells. For the body to sustain long-term immunity against illness, they are crucial.
A person’s CD4+ T cell count may aid in HIV diagnosis. This virus enters CD4+ T cells directly and multiplies there. The immune system’s capacity to fend off additional infections is weakened when the virus steadily kills CD4+ T cells as it multiplies.
Memory CD4 T Lymphocyte Cells
Memory CD4+ T-cells are helpful for preserving one’s immune system. They develop from naïve CD4+ T-cells, which are the building blocks of memory cells, and have the ability to identify and target pathogens the body has previously met. Yet, the body responds more quickly and forcefully the second time it comes into contact with the germ.
Types of CD4+ cells
There are several subtypes of CD4+ T cells, and each has a unique purpose. There are three main subsets:
- T helper cell 1 (TH1)
- T helper cell 2 (TH2)
- T helper cell 17 (TH17)
- Regulatory T cells (Treg)
- Follicular Helper (Tfh) T Cells
- T helper cell 9 (TH9)
T helper cell 1 (TH1):
They coordinate immune reactions to pathogens that live within cells, such bacteria. Cytokines are proteins that can influence the immune system or obliterate infections directly and are produced by TH1. The following are examples of cytokines produced by TH1: Interleukin-2, tumor necrosis factor beta, and interferon-gamma.
T helper cell 2 (TH2)
They coordinate immune reactions to pathogens that live body’s cells, for example, helminths, which are parasitic worms.Furthermore, cytokines produced by TH2 stimulate other lymphocytes and modulate allergic responses. Among the cytokines that TH2 generates are: interleukin 4, 5, and 13
T helper cell 17 (TH17)
They generate the signaling chemical interleukin 17, which causes other immune cells to become active. TH17 aids in defending the body against fungus and bacteria that live outside of the body’s cells.
Regulatory T cells (Treg)
These regulatory T cells monitor on and control other immune reactions, assisting in the prevention of autoimmune conditions and preserving homeostasis.
Follicular Helper (Tfh) T Cells
Tfh are C-X-C motif receptor-5 (CXCR 5+) expressing cells found in lymphoid tissue’s follicular regions, where they take role in the production of B lymphocytes that are specific to antigens.
Tfh cells have been categorized as Tfh1, Tfh2, and Tfh10 depending on the major cytokine produced. Tfh1 encourages the synthesis of IgG2a by secreting IFN. IgG1 and IgE are more likely to be produced when Tfh2 secretes IL4. Tfh10 promotes IgA secretion by secreting IL10.
T helper cell 9 (TH9)
It was discovered that TGF- β redirected Th2 differentiation to Th9 cell formation. Moreover, TGF- β directly stimulates the development of Th9 cells when combined with IL 4. IRF4 also contributes significantly.
CD4 Count and HIV
We can assess a person’s immune system activity by counting the number of active CD4 cells that are present in the blood. The CD4 count, a quick blood test, determines how many functional CD4 cells are present in a cubic millimeter of blood. The immune system functions better when the CD4 level is greater.
Depending on the community, age group, etc., a healthy adult’s normal CD4 count can vary greatly, but is normally between 500 and 1,500 cells per cubic millimeter of blood (mL). But, when it goes below 200, the condition is officially categorized as AIDS (acquired immune deficiency syndrome).
Normal CD4 count
For healthy adults and teenagers, the normal CD4 count ranges from 500 to 1,200 cells per cubic millimeter.
Low CD4 Count
Below 500 cells per cubic millimeter is a low CD4 level.
You have AIDS if your CD4 count is 200 or less cells per cubic millimeter. You have a significant risk of contracting cancer or life-threatening illnesses if you have AIDS.
A low CD4 count may be brought on by an infection even if you do not have HIV. Low CD4 numbers can also result from immune system sabotaging drugs and cancer treatment. A low CD4 count might occasionally have unknown causes, however this is rare.
High CD4 Count:
Levels that are higher than usual might indicate an infection or blood malignancy.
HIV must grow in order to be able to infect host cells, as CD4 cells are its main target.
During infections, HIV binds to these cells and releases its genetic material, changing the host’s genetic makeup and ultimately producing HIV virions. The host’s CD4 cells are obliterated in the process. As a result, these individuals’ ability to elicit protective immunological responses decreases, eventually getting to the point where the body is vulnerable to opportunistic infections.
What is the difference between CD4 and CD8 T cells?
They both function in immune response but differ in the presence of surface protein, presence of pathogens and function.
CD4+ T cells have the ability to initiate and direct an immunological response. They identify pathogens and release cytokines that stimulate other immune cells, such as CD8+ T cells, to become active. They do not, however, directly engage in the attack or eradication of diseases.
Contrarily, CD8+ T lymphocytes directly combat infections and malignant cells by attaching to them and secreting poisonous chemicals that obstruct pathogen replication and result in cell death. Also, they are referred to as cytotoxic T-cells or cytotoxic lymphocytes.
Learn More
References
- https://www.frontiersin.org/articles/10.3389/fimmu.2022.867189/full
- https://medlineplus.gov/lab-tests/cd4-lymphocyte-count/
- https://clinicalinfo.hiv.gov/en/glossary/cd4-t-lymphocyte
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312336/
- https://www.webmd.com/hiv-aids/cd4-count-what-does-it-mean
- https://www.verywellhealth.com/what-are-cd4-t-cells-49354
- https://www.medicalnewstoday.com/articles/cd4-t-cells#vs-cd-8-t-cells
- https://www.thewellproject.org/hiv-information/understanding-cd4-cells-and-cd4-cell-tests
- https://byjus.com/neet/cd4-cells/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2679806/