What are Fluoroquinolones?
Fluoroquinolones are a class of antibiotics that are commonly used to treat bacterial infections. They work by inhibiting bacterial DNA synthesis, which ultimately leads to the death of the bacteria. These antibiotics are often prescribed to treat a variety of infections, such as urinary tract infections, respiratory tract infections, and skin infections.
Examples include ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin, and ofloxacin. These antibiotics are usually available in oral or intravenous forms.
General structure of fluoroquinolones
- Fluoroquinolones have a quinoline ring system with one or more fluorine atoms attached.
- The quinoline ring system is composed of two fused six-membered rings with nitrogen atoms at positions 1 and 4.
- Fluorine atoms are usually located at positions 6 and/or 8 of the quinoline ring system.
- Fluoroquinolones typically have a carboxylic acid group at position 3.
- They also have a nitrogen-containing heterocyclic ring at position 7.
- The specific structure of the heterocyclic ring can vary depending on the particular fluoroquinolone.
- The presence of the fluorine atoms in the structure of fluoroquinolones enhances their antibacterial activity and increases their ability to penetrate bacterial cells.
Classification of Quinolone Antibiotics
Fluoroquinolones are a class of antibiotics used to treat bacterial infections. These drugs work by blocking the synthesis of bacterial DNA, leading to cell death. The new quinolone antibiotic classification takes into consideration the extended antibacterial spectrum of the newer fluoroquinolones as well as their clinical applications.
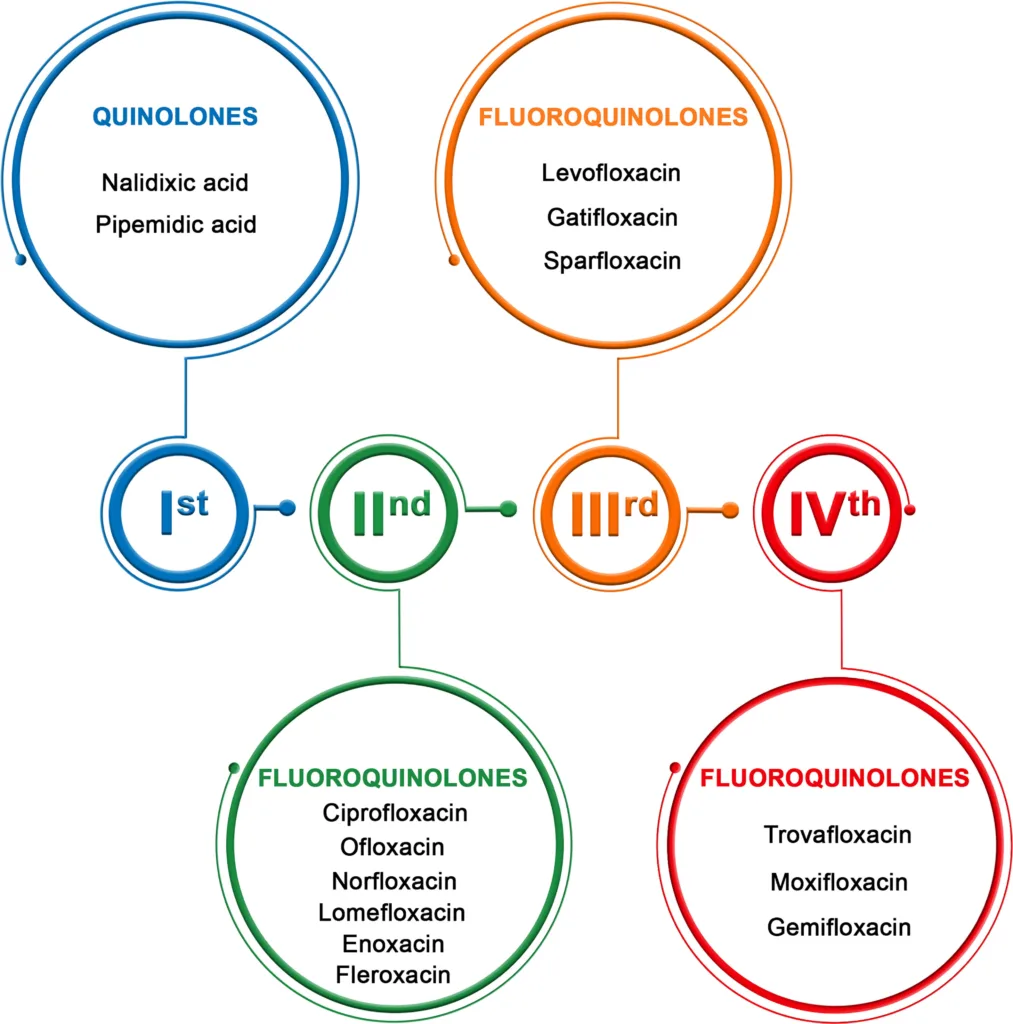
First generation fluoroquinolones
The first generation includes cinoxacin and nalidixic acid. These drugs are less commonly used today due to minimal serum levels and increased risk of bacterial resistance. They are only recommended for uncomplicated urinary tract infections and not for patients with poor renal function.
Second-generation fluoroquinolones
Second-generations have increased gram-negative activity and broad clinical applications for complicated urinary tract infections, sexually transmitted diseases, pneumonias, and skin infections. Examples of second-generation drugs include ciprofloxacin, enoxacin, lomefloxacin, norfloxacin, and ofloxacin. Ciprofloxacin is particularly effective against P. aeruginosa and can treat osteomyelitis caused by susceptible organisms. Ofloxacin has greater activity against Chlamydia trachomatis.
Third generation fluoroquinolones
The third generation, including levofloxacin, gatifloxacin, moxifloxacin, and sparfloxacin, have expanded activity against gram-positive organisms, particularly penicillin-sensitive and penicillin-resistant S. pneumoniae, and atypical pathogens such as Mycoplasma pneumoniae and Chlamydia pneumoniae. They are useful in the treatment of community-acquired pneumonia, acute sinusitis, and acute exacerbations of chronic bronchitis, and for urinary tract infections and gonorrhea. Gatifloxacin carries a risk of phototoxicity and prolongation of the QT interval.
Fourth generation fluoroquinolones
The fourth generation, represented by trovafloxacin, adds significant antimicrobial activity against anaerobes while maintaining broad-spectrum gram-positive and gram-negative coverage. Trovafloxacin is available in oral and intravenous formulations, but it is reserved for life- or limb-threatening infections requiring inpatient treatment and should not be taken for longer than 14 days due to the risk of hepatotoxicity.
Mechanism of Action
- Fluoroquinolones act by inhibiting bacterial DNA synthesis.
- They bind to and interfere with DNA gyrase and topoisomerase IV enzymes, which are essential for DNA replication, transcription, and repair in bacteria.
- Inhibition of these enzymes leads to the accumulation of DNA damage, breakage, and cell death in susceptible bacteria.
- Fluoroquinolones are bactericidal and exhibit concentration-dependent killing, meaning higher drug concentrations result in greater bacterial killing.
- They have broad-spectrum activity against both gram-positive and gram-negative bacteria, as well as atypical pathogens.
- Fluoroquinolones penetrate well into tissues and body fluids, making them effective for the treatment of various infections.
Antimicrobial activity of Fluoroquinolones
Fluoroquinolones have broad-spectrum antimicrobial activity against both Gram-positive and Gram-negative bacteria, as well as atypical pathogens such as Mycoplasma, Legionella, and Chlamydia. They exert their bactericidal effects by inhibiting DNA gyrase and topoisomerase IV enzymes, which are essential for DNA replication and transcription. This inhibition leads to the formation of double-stranded breaks in the bacterial DNA, eventually causing cell death.
The antimicrobial spectrum of fluoroquinolones is influenced by their chemical structure, pharmacokinetic properties, and ability to penetrate different tissues.
First-generation fluoroquinolones have limited activity against Gram-negative bacteria and are mainly used for treating uncomplicated urinary tract infections.
Second-generation fluoroquinolones have increased Gram-negative coverage and are useful for treating more complicated infections such as pneumonia, bone and joint infections, and sexually transmitted diseases.
Third-generation fluoroquinolones have expanded activity against Gram-positive organisms, including penicillin-resistant Streptococcus pneumoniae, and are used for treating community-acquired pneumonia, sinusitis, and exacerbations of chronic bronchitis.
Fourth-generation fluoroquinolones, such as trovafloxacin, have additional activity against anaerobic bacteria.
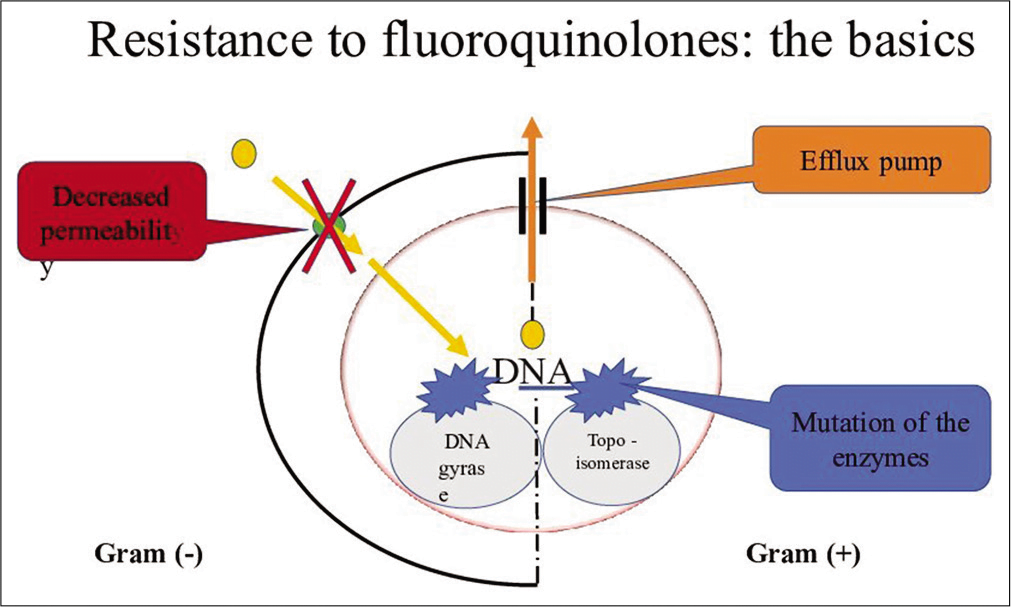
Mechanism of Resistance Development
Fluoroquinolone resistance can occur through various mechanisms, including:
- Target site mutations: Resistance can occur due to mutations in the DNA gyrase and topoisomerase IV genes, which are the targets of fluoroquinolones. These mutations can prevent the binding of the drug to its target site.
- Efflux pumps: Some bacteria have efflux pumps that can remove the antibiotic from the bacterial cell before they can cause damage. This reduces the concentration of the drug within the cell, making it less effective.
- Plasmid-mediated resistance: Resistance can also occur through the transfer of plasmids containing genes that produce enzymes such as aminoglycoside acetyltransferases or adenyltransferases. These enzymes can modify the fluoroquinolone molecule, making it less effective or inactive.
- Decreased permeability: Some bacteria can reduce their permeability to fluoroquinolones by altering their cell wall structure or producing porins that limit the entry of the drug into the cell.
- Biofilm formation: Bacteria within biofilms can be highly resistant to antibiotics, including fluoroquinolones. This is because the biofilm matrix can physically protect the bacteria from the drug, making it difficult for the drug to reach the cells within the biofilm.
- Overuse and misuse of antibiotics: Overuse and misuse of antibiotics, including fluoroquinolones, can lead to the development and spread of resistant bacteria.
Adverse effects of Fluoroquinolones
Fluoroquinolones can cause a range of adverse effects, some of which can be serious. Here are some of the adverse effects associated with fluoroquinolones:
- Gastrointestinal effects: The most common side effects of fluoroquinolones are gastrointestinal, including nausea, vomiting, diarrhea, and abdominal pain.
- CNS effects: Fluoroquinolones can cause CNS side effects, such as headache, dizziness, and confusion. Rarely, seizures and hallucinations can occur.
- Tendon rupture: They can cause tendon rupture, especially in the Achilles tendon. This adverse effect is more common in older adults and people taking corticosteroids.
- QT prolongation: Fluoroquinolones can prolong the QT interval, which can lead to serious cardiac arrhythmias, including torsades de pointes.
- Photosensitivity: Some of these antibiotic can cause photosensitivity, making the skin more sensitive to sunlight and increasing the risk of sunburn and rash.
- Hypersensitivity reactions: They can cause hypersensitivity reactions, including anaphylaxis, angioedema, and Stevens-Johnson syndrome.
- Other effects: Other adverse effects include liver toxicity, renal failure, blood glucose disturbances, and peripheral neuropathy.
It is crucial to note that the occurrence and severity of these side effects might vary depending on the fluoroquinolone, dose, and length of therapy. Patients using these antibiotics should be monitored for these side effects and urged to notify their healthcare practitioner if any new or worsening symptoms occur.
Warning: This article is intended for educational and research purposes only, not for clinical application.