Immunity can be defined as a complex biological system or defense mechanism of a self-providing capacity to recognize and tolerate foreign particle within body system which maybe natural (by birth) or acquired. Herd immunity (an acquired immunity) is a key concept for epidemic control. Herd immunity can be defined as the immunity of self to population at which disease spreading will decline or stop even if preventive measures are relaxed.
What is Acquired Immunity?
Acquired immunity develops later in an individual, either through natural infection with a pathogen or through immunization with a vaccine.
Herd Immunity
Herd immunity (an acquired immunity) is a key concept for epidemic control. Herd immunity can be defined as the immunity of self to population at which disease spreading will decline or stop even if preventive measures are relaxed. Herd immunity starts from the effects from individual immunity scaled to the level of the population. Thus, in a simple term, it refers to the indirect protection from infection to susceptible individuals when a sufficiently large proportion of immune individuals exist in a population. This population-level effect is often considered in the context of vaccination programs, which aim to establish herd immunity so that those who cannot be vaccinated, including the very young and immunocompromised, are still protected against disease.
An example of herd immunity in the population, can be analyzed from measles. If 95% of the people to have immunity or antibodies against measles virus after proper vaccination, even if you have 5% of children not vaccinated, these others actually have enough protection in the population to prevent the measles virus from actually going from one person to the next. Thus, herd immunity is population immunity acting as a barrier of people who are protected, who break that chain of transmission such that every single person in the area, in the population, to necessarily be protected.
For herd immunity, at least 50 to 70% of the population to have immunity to break the chain of transmission known as the threshold population which can resist the infection. If we allow this to happen naturally, it will take a long time, of course, but more importantly, it’s going to do a lot of collateral damage.As,the introduction of an infected individual depends on the prevalence of existing immunity to a pathogen in a population leading to different outcomes. In a completely naive population, a pathogen will propagate through susceptible hosts in an unchecked manner increasing infected individuals. However, if a fraction of the population has immunity to that same pathogen, an effective contact between infected and susceptible hosts is reduced. When many hosts are immune the transmission of the pathogen is halted and its prevalence will decline protecting the susceptible hosts too. The point at which the proportion of susceptible individuals falls below the threshold needed for transmission is known as the herd immunity threshold. The herd immunity begins to take effect only above this level or threshold and finally, susceptible individuals can be benefited from indirect protection from infection.
Learn more about
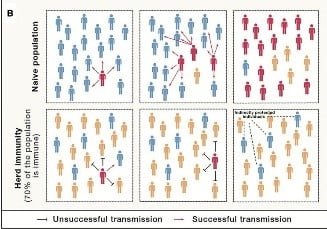
[Source; Randolph HE, Barreiro LB. Herd Immunity: Understanding COVID-19. Immunity. 2020;52(5):737-741, Figure 1]
In the above figure, in the naive population as we can observe has an outbreak that quickly emerges whereas in the scenario of herd immunity, the chain is broken due to immunity acquired after the threshold infection. Thus the virus fails to spreads and persist in the population.
The COVID-19 and the herd immunity?
Is it the natural vaccine for coronavirus disease 2019 (Covid-19) ?
Coronavirus disease 2019 (COVID-19), is an infectious disease with high respiratory pathogenicity, caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).It was emerged in December 2019 in Wuhan, China, which eventually transmitted across the globe being a major pandemic. According to the John Hopkin’s Corona Resource Center, the disease has infected more than 29.0 million people across 215 countries and territories as on September 16, 2020.
For COVID-19, which has an estimated infection fatality ratio of 0.3–1.3%, the cost of reaching herd immunity through natural infection would be very high, especially in the absence of improved patient management and without optimal shielding of individuals at risk of severe complications. An optimistic herd immunity is assumed to be threshold of 50%, for countries. So in a bigger picture, even if 1% of people who get infection are ultimately going to die, then this can add up to a huge number of people, if we look at the global population.
In addition to this, immunocompromised person, older individuals and those with comorbidities are disproportionally affected, with infection of COVID and the fatality ratios of 3.3% for those older than 60 years. There is also increased mortality in individuals with chronic diseases such as diabetes, cardiac disease, chronic respiratory disease or obesity though the expected impact would be substantially smaller in younger populations. And that is why it’s not a good idea to try to achieve herd immunity by just letting the infection transmission and the need of a vaccine.
For the establishment herd immunity, the immunity generated by vaccination or natural infection is therefore necessary but it must prevent onward transmission, not just clinical disease. For pathogens in which lifelong immunity is induced, as is the case for measles vaccination or infection, herd immunity is highly effective and can prevent pathogen spread within a population. However, this situation may be relatively rare, as immunity for many other infectious diseases, such as pertussis and rotavirus, wanes over time. So, there lies a challenge in case of COVID-19 as herd immunity is less effective, and periodic outbreaks can still occur.
The safest way to reach herd immunity is an effective vaccine. As, of August 2020, six anti-SARS-CoV-2 vaccines have reached phase 3 trials, so it may be accessible by early 2021, although their safety and efficacy remains to be established. As long as the assembly and delivery of a vaccine will initially be limited, it’ll be important to prioritize highly exposed populations and people in danger of severe morbidity.
Thus, summing up there are two possible approaches to build widespread SARS-CoV-2 immunity:
(1) Besides providing individual protection, vaccination programs should run parallelly aiming for so-called population or herd immunity, i.e., immunization of a large proportion of the population to protect the non-vaccinated, immunologically naive, and immunocompromised individuals by reducing the percentage of vulnerable hosts to a level below the transmission threshold, a mass vaccination campaign, which requires the development of an effective and safe vaccine.
(2) Natural immunization of global populations with the virus over time—a large fraction of the human population would need to become infected with the virus, and finally adapt to it. Thus, in the absence of a vaccination program, establishing herd immunity should not be the ultimate goal.
References
- Fontanet, A., Cauchemez, S. COVID-19 herd immunity: where are we?. Nat Rev Immunol (2020). https://doi.org/10.1038/s41577-020-00451-5
- Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. 2020;369(6505):846-849. https://science.sciencemag.org/content/369/6505/846.abstract
- Randolph HE, Barreiro LB. Herd Immunity: Understanding COVID-19. Immunity. 2020;52(5):737-741. https://doi.org/10.1016/j.immuni.2020.04.012
- Frederiksen LSF, Zhang Y, Foged C, Thakur A. The Long Road Toward COVID-19 Herd Immunity: Vaccine Platform Technologies and Mass Immunization Strategies. Front Immunol. 2020;11:1817. Published 2020 Jul 21. https://www.frontiersin.org/articles/10.3389/fimmu.2020.01817/full
- Kwok KO, Lai F, Wei WI, Wong SYS, Tang JWT. Herd immunity – estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect. 2020;80(6):e32-e33. doi:10.1016/j.jinf.2020.03.027
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-1
- https://newseu.cgtn.com/news/2020-09-14/Does-Sweden-s-COVID-19-experience-support-the-herd-immunity-theory–TL82pOjfpe/index.html
- https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1?
- https://coronavirus.jhu.edu/map.html