Heart failure is a prevalent and complex condition that affects millions of individuals globally. This comprehensive guide provides an in-depth understanding of heart failure, including its definition, causes, symptoms, treatment options, and impact on different populations. Whether you’re seeking information for yourself or a loved one, this guide aims to equip you with a thorough understanding of this critical health condition.
Overview of Heart Failure
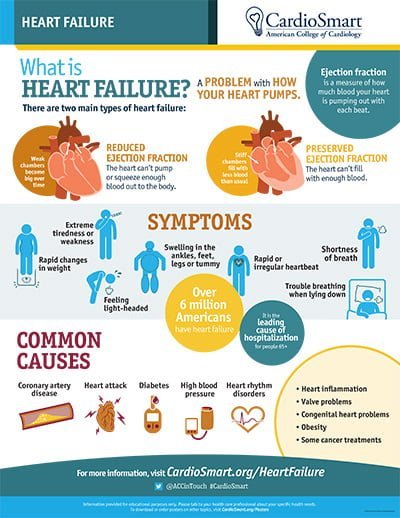
Heart failure is a serious medical condition where the heart is unable to pump blood efficiently to meet the body’s needs. This inefficiency can lead to a build-up of fluid in the lungs and other tissues, causing symptoms such as shortness of breath, fatigue, and swelling. The heart failure can result from various underlying health issues, and understanding its nature is crucial for effective management and treatment.
Definition
Heart failure, also referred to as congestive heart failure (CHF), is a state where the heart’s ability to pump blood is compromised. It doesn’t mean the heart has stopped working but rather that it is struggling to function effectively. This can occur due to the heart’s inability to contract properly (systolic heart failure) or its inability to relax and fill with blood correctly (diastolic heart failure). As a result, blood may back up in the lungs or other parts of the body, leading to various symptoms and complications.
How Does the Normal Heart Work?
To understand heart failure, it’s essential to comprehend how a healthy heart functions. The heart is a muscular organ divided into four chambers:
- Right Atrium: Receives deoxygenated blood from the body through the superior and inferior vena cavae.
- Right Ventricle: Pumps the deoxygenated blood to the lungs via the pulmonary arteries for oxygenation.
- Left Atrium: Receives oxygenated blood from the lungs through the pulmonary veins.
- Left Ventricle: Pumps oxygen-rich blood to the rest of the body through the aorta.
In a healthy heart, this process is highly coordinated. The heart’s chambers contract and relax in a precise sequence to maintain a consistent blood flow and pressure throughout the body. The right side of the heart handles blood flow to the lungs, while the left side manages blood flow to the rest of the body. This efficient circulation ensures that oxygen and nutrients are delivered to tissues and organs, and waste products are removed.
Heart Failure Treatment
Effective treatment of heart failure involves a multi-faceted approach designed to manage symptoms, improve quality of life, and address the underlying causes. Treatment strategies typically include lifestyle modifications, medications, and, in some cases, surgical interventions.
Lifestyle Modifications
- Diet: Adopting a heart-healthy diet is crucial. This typically involves reducing salt (sodium) intake to prevent fluid retention, eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, and limiting saturated fats and cholesterol.
- Exercise: Regular physical activity can strengthen the heart and improve overall cardiovascular health. It’s essential to engage in moderate exercise, as advised by a healthcare professional, to avoid overexertion.
- Weight Management: Maintaining a healthy weight helps reduce the heart’s workload and can alleviate symptoms. Obesity can exacerbate heart failure, so weight loss through diet and exercise is often recommended.
- Quit Smoking: Smoking is a major risk factor for heart disease and can worsen heart failure. Quitting smoking improves overall cardiovascular health and supports heart function.
- Limit Alcohol: Excessive alcohol consumption can exacerbate heart failure. Moderation is key, and individuals with heart failure should follow their doctor’s recommendations regarding alcohol intake.
Medications
Medications play a crucial role in managing heart failure. They help to alleviate symptoms, improve heart function, and prevent progression. Commonly prescribed medications include:
- ACE Inhibitors: These drugs, such as enalapril and lisinopril, help to relax blood vessels, reduce blood pressure, and decrease the heart’s workload.
- Beta-Blockers: Medications like metoprolol and carvedilol reduce heart rate and blood pressure, which can improve heart function and reduce symptoms.
- Diuretics: These help to reduce fluid retention by increasing urine output. Common diuretics include furosemide and hydrochlorothiazide.
- Aldosterone Antagonists: Drugs like spironolactone and eplerenone help to reduce fluid build-up and improve heart function.
- Digoxin: This medication increases the force of heart contractions and helps control the heart rate, particularly in patients with atrial fibrillation.
Surgical and Device-Based Interventions
In severe cases of heart failure, surgical procedures and implanted devices may be necessary:
- Heart Valve Surgery: Repairing or replacing damaged heart valves can improve blood flow and reduce symptoms.
- Coronary Artery Bypass Grafting (CABG): This procedure helps to restore blood flow to the heart by bypassing blocked arteries.
- Implantable Cardioverter-Defibrillators (ICDs): These devices monitor heart rhythms and deliver electrical shocks if dangerous arrhythmias are detected.
- Cardiac Resynchronization Therapy (CRT): This treatment involves implanting a special pacemaker that coordinates the heart’s contractions, improving its efficiency.
- Left Ventricular Assist Devices (LVADs): These mechanical pumps help the heart pump
blood more effectively and are often used in advanced cases of heart failure or as a bridge to a heart transplant.
Heart Failure Symptoms
Heart failure symptoms can significantly impact daily life and vary in severity. Recognizing these symptoms early is crucial for effective management and treatment.
Common Symptoms
- Shortness of Breath: This can occur during physical activity or even at rest. Individuals with heart failure may experience difficulty breathing when lying flat, known as orthopnea, or may have difficulty breathing at night, known as paroxysmal nocturnal dyspnea.
- Fatigue: A prevalent symptom, fatigue in heart failure can be overwhelming, making it challenging to perform everyday activities. This is due to the heart’s reduced ability to pump sufficient blood and oxygen to the body’s tissues.
- Swelling: Fluid retention often leads to swelling, particularly in the legs, ankles, and feet. This can also extend to the abdomen (ascites) and can result in weight gain due to fluid accumulation.
- Persistent Cough: A cough that doesn’t go away, often accompanied by frothy or blood-tinged sputum, can be a sign of fluid in the lungs due to heart failure.
- Rapid or Irregular Heartbeat: Individuals with heart failure may experience palpitations, which are sensations of rapid or irregular heartbeats. This can be uncomfortable and alarming.
Heart Failure Symptoms in Men and Women
Heart failure symptoms can manifest differently in men and women. Understanding these differences can aid in early diagnosis and treatment.
- In Men: Symptoms often include classic signs such as shortness of breath, fatigue, and swelling in the lower extremities. Men may also experience chest discomfort or pain.
- In Women: Women may experience symptoms that are less commonly associated with heart failure, such as nausea, loss of appetite, and gastrointestinal symptoms. They may also report increased fatigue and shortness of breath even with minimal exertion. Women are more likely to experience symptoms that overlap with other conditions, making diagnosis more challenging.
Heart Failure Causes
Understanding the causes of heart failure is essential for effective prevention and treatment. Several conditions and factors can contribute to heart failure:
Coronary Artery Disease (CAD)
Coronary artery disease is one of the most common causes of heart failure. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to atherosclerosis. This reduced blood flow can damage the heart muscle, leading to heart failure.
High Blood Pressure (Hypertension)
Chronic high blood pressure puts extra strain on the heart, causing it to work harder to pump blood. Over time, this can lead to thickening of the heart muscle (left ventricular hypertrophy) and ultimately heart failure.
Heart Valve Disorders
Heart valves regulate blood flow through the heart. Disorders such as stenosis (narrowing of the valve) or regurgitation (leaking of the valve) can impair heart function and contribute to heart failure. Conditions like mitral valve prolapse or aortic stenosis are examples of valve disorders that can lead to heart failure.
Myocarditis
Myocarditis is inflammation of the heart muscle, often caused by viral infections. This inflammation can weaken the heart and impair its ability to pump blood, leading to heart failure.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle that affect its size, shape, and function. This can include dilated cardiomyopathy (where the heart becomes enlarged and weakened), hypertrophic cardiomyopathy (where the heart muscle becomes abnormally thick), and restrictive cardiomyopathy (where the heart muscle becomes rigid and less flexible).
Diabetes
Diabetes increases the risk of developing heart failure due to the damaging effects of high blood sugar levels on blood vessels and nerves. People with diabetes are more likely to develop coronary artery disease and high blood pressure, which can lead to heart failure.
Types of Heart Failure
Heart failure can be classified based on the side of the heart affected and the heart’s pumping function. The two primary types are:
Left-Sided Heart Failure
Left-sided heart failure occurs when the left side of the heart is unable to pump blood effectively to the rest of the body. This type can be further categorized into:
- Systolic Heart Failure: Also known as heart failure with reduced ejection fraction (HFrEF), it is characterized by the heart’s reduced ability to contract and pump blood. The ejection fraction (EF) is a measurement of how much blood the left ventricle pumps out with each contraction. In systolic heart failure, this percentage is lower than normal.
- Diastolic Heart Failure: Also known as heart failure with preserved ejection fraction (HFpEF), it occurs when the heart’s ability to relax and fill with blood is impaired. The ejection fraction may remain normal, but the heart muscle is stiff and less compliant, affecting the heart’s ability to fill with blood.
Right-Sided Heart Failure
Right-sided heart failure occurs when the right side of the heart is unable to pump blood effectively to the lungs for oxygenation. This often results from left-sided heart failure but can also occur due to lung diseases or conditions affecting the right side of the heart directly. Symptoms include swelling in the legs, abdomen, and feet, and can be accompanied by fluid build-up in these areas.
Congestive Heart Failure (CHF)
Congestive heart failure is a term used to describe the condition where fluid accumulates in the lungs and other tissues due to the heart’s impaired ability to pump blood efficiently. This term is often used interchangeably with heart failure but specifically highlights the fluid retention aspect.
4 Stages of Congestive Heart Failure
Heart failure is categorized into four stages, each representing the severity of the condition and the degree of symptoms experienced.
Stage A
In this stage, individuals are at high risk for developing heart failure due to risk factors such as hypertension, diabetes, or a family history of heart disease. However, there are no apparent symptoms or structural heart changes at this stage.
Stage B
Stage B involves structural changes to the heart, such as left ventricular hypertrophy or previous heart attacks, but without noticeable symptoms. Individuals may have a diagnosis of heart disease but do not yet experience symptoms of heart failure.
Stage C
At this stage, individuals experience symptoms of heart failure. Symptoms such as shortness of breath, fatigue, and swelling become apparent. The heart’s function is impaired, and daily activities may be limited due to these symptoms.
Stage D
Stage D represents advanced heart failure, where symptoms are severe and persistent despite treatment. Individuals may require specialized treatments such as mechanical support devices, heart transplantation, or palliative care.
Signs of Worsening Heart Failure in Older Adults
In older adults, heart failure can present differently and may worsen gradually. Recognizing signs of worsening heart failure is crucial for timely intervention and management.
Increased Shortness of Breath
Older adults may notice increased difficulty breathing, even with minimal exertion or while lying flat. This can indicate worsening fluid build-up in the lungs or a deterioration in heart function.
Severe Swelling
Significant swelling in the legs, ankles, and feet, or noticeable abdominal swelling (ascites), can be signs of worsening heart failure. This fluid retention may lead to rapid weight gain.
Confusion or Memory Issues
Reduced blood flow to the brain can result in cognitive symptoms such as confusion, memory issues, or difficulty concentrating. These symptoms can indicate worsening heart failure and reduced overall health.
Rapid Weight Gain
Sudden or rapid weight gain due to fluid retention can be a sign of worsening heart failure. Monitoring weight regularly and reporting any significant changes to a healthcare provider is essential.
Persistent Fatigue
A marked increase in fatigue, where daily activities become challenging, can indicate that heart failure is progressing. This can result from the heart’s reduced ability to pump blood effectively and provide sufficient oxygen to the body.
Early Signs of Heart Failure in Older Adults
Early recognition of heart failure in older adults can improve outcomes and facilitate early intervention.
Mild Shortness of Breath
Early signs may include mild shortness of breath during activities that were previously manageable. This can be an early indicator of heart failure and warrants evaluation by a healthcare provider.
Increased Fatigue
Older adults may experience increased fatigue, feeling unusually tired or weak during daily activities. This symptom can be subtle but is an important early sign of heart failure.
Subtle Swelling
Early swelling may be observed in the ankles or legs, which can be subtle at first but should be monitored. Fluid retention in these areas can be an early sign of heart failure.
Frequent Urination
Increased frequency of urination, particularly at night (nocturia), due to fluid build-up can be an early sign of heart failure. This is often related to the body’s attempt to manage fluid overload.
Systolic Heart Failure
Systolic heart failure, or heart failure with reduced ejection fraction (HFrEF), is characterized by the heart’s reduced ability to contract and pump blood. Key aspects of systolic heart failure include:
Reduced Ability to Pump Blood
The heart’s left ventricle is weakened and unable to pump blood efficiently. This leads to reduced ejection fraction, which is a measurement of the percentage of blood ejected from the heart with each beat.
Symptoms
Individuals with systolic heart failure may experience symptoms such as shortness of breath, fatigue, and fluid retention. These symptoms occur due to the heart’s inability to effectively pump blood to meet the body’s needs.
Heart Failure Medications
Medications are a cornerstone of heart failure management, helping to control symptoms, improve heart function, and prevent progression. Key medications used in heart failure include:
ACE Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors, such as enalapril, lisinopril, and ramipril, help to relax blood vessels, reduce blood pressure, and decrease the heart’s workload. They are effective in improving symptoms and slowing the progression of heart failure.
Beta-Blockers
Beta-blockers, including metoprolol, carvedilol, and bisoprolol, work by reducing the heart rate and blood pressure. This helps the heart pump more efficiently and reduces the strain on the heart muscle.
Diuretics
Diuretics, such as furosemide and hydrochlorothiazide, help to eliminate excess fluid from the body by increasing urine output. This reduces swelling and fluid build-up, improving symptoms of heart failure.
Aldosterone Antagonists
Aldosterone antagonists, including spironolactone and eplerenone, help to reduce fluid retention and improve heart function by blocking the effects of aldosterone, a hormone that promotes sodium and water retention.
Digoxin
Digoxin increases the force of heart contractions and helps control heart rate, particularly in individuals with atrial fibrillation. It can improve symptoms and overall heart function in patients with heart failure.
Conclusion
Heart failure is a complex and multifaceted condition that requires a comprehensive approach to management. Understanding its definition, symptoms, causes, and treatments is essential for effective care and improving quality of life. Whether through lifestyle modifications, medications, or advanced interventions, managing heart failure effectively can lead to better outcomes and enhanced well-being. If you or a loved one are experiencing symptoms of heart failure or have been diagnosed with the condition, it is crucial to work closely with healthcare professionals to develop a tailored treatment plan that addresses individual needs and preferences.